Share
1
item
избран
Получете достъп до изключителни дерматологични услуги, за да подобрите своите професионални знания: над 500 визуални материала за патологии, клинични случаи и експертни видеа
Възползвайте се от ценни функции: аудио слушане, материали за споделяне с вашите пациенти
Бъдете информирани за предстоящи събития и уебинари, последни научни публикации и продуктови иновации
Вече имате профил? Влезте тук
Reports written by Dr. Joël Claveau (Dermatologist, Quebec), Prof. Brigitte Dréno (Dermatologist, France), Dr. Ben Esdaile (Dermatologist, United Kingdom), Dr. Ricardo Limongi (Dermatologist, Brazil) and Dr. Rémi Maghia (Dermatologist, France)
Related topics
Speakers: Prof. Aimilios Lallas, Dr. Wilhelm Stolz and Dr. Susana Puig
Report written by Dr. Joël Claveau
Challenging Cases of Dermoscopy & Dermoscopy in 2022
Historically, dermatologists in North America used dermoscopy less than those in Europe. However, this technique, which is essential in diagnosing a variety of skin lesions, is now being taught in a number of residency programmes in North America and is also being discussed at key congresses. This year, there were ten or so dermoscopy sessions at the American Academy of Dermatology’s Annual Meeting which was held in Boston last week. Below is a summary of some of the conferences.
First, I had the opportunity to run an interactive dermoscopy workshop with Greek dermatologist Aimilios Lallas. He presented the signs evocative of squamous cell carcinoma of the lips. The clinical signs are an advanced age, presence of an exophytic lesion, a hyperkeratotic appearance and its location on the lower lip. Dermoscopic signs include the presence of ulceration and whitish globules (“white clouds”). This helps us differentiate carcinoma from actinic cheilitis and inflammatory conditions such as lichen planus. He then presented the dermoscopic signs of blue naevus. It usually presents as a stable, old lesion with an even, bluish or brownish pattern covering 75% of the lesion, with no blood vessels. For the differential diagnosis, we should consider cutaneous metastasis of melanoma, especially if the patient has had a nearby melanoma excised. He discussed the dermoscopic signs of combined naevi, i.e. the combination of a globular or reticulated naevus with a bluish, even zone. He finished with examples of the dermoscopic signs of a few common inflammatory conditions: psoriasis (punctiform vessels), dermatitis (scales and yellowish scabs), lichen planus (Wickham striae), pityriasis rosea (collarette) and scabies (“jet with contrail” signs).
In my part, I reiterated the importance of a systematic approach in dermoscopy, as seen with the 2- step algorithm. This approach ensures we first recognise melanocytic lesions (naevus vs melanoma) if we observe a melanocytic pattern (reticulated network, globular or even pattern). If no pattern is visible, we must consider the main non-melanocytic lesions: seborrhoeic keratosis, dermatofibroma, angioma, basal cell and squamous cell carcinomas. For melanocytic lesions, I summarised the main signs of melanomas that should be recognised (atypical network, atypical striae, irregular globules and dots, shiny white striae, reversed network, signs of regression and a bluish-grey veil). It is important that we observe atypical and heterogeneous vessels in hypopigmented or achromic melanomas. We revised the classic patterns of benign naevi: evenly reticulated, reticulated in areas, globular, combination of reticulation, globules, and even areas. I ended with a presentation of a few dermoscopic signs of melanoma on unusual anatomic sites: face (irregular pseudo-network with annular granular pattern, rhomboidal structures and obstructed follicles), acral skin (ridge pattern) and nails (different-coloured uneven longitudinal bands).
In an excellent conference on the dermoscopic signs of rare tumours, Dr Wilhelm Stolz presented the signs of Merkel cell carcinoma. We can observe reddish areas, shiny whitish striae, and polymorphic blood vessels which may have branching. Merkel cell carcinoma can mimic basal cell carcinoma.
Other tumours which can resemble basal cell carcinoma include trichoepithelioma (branching telangiectasias with yellowish microcysts and comedo-like globules) and sebaceous adenoma, often in Muir-Torre syndrome (branching telangiectasias and round, yellowish structures). For a differential diagnosis with haemangioma, nodular melanoma or even pigmented basal cell carcinoma, we must consider Kaposi sarcoma with its dermoscopic rainbow pattern which is found on the edge of saccular vascular structures. A reddish, non-specific nodule with polymorphic blood vessels visible on scoping may well be cutaneous metastasis of various adenocarcinoma, typically adenocarcinoma of the kidney.
The last conference that I would like to summarise is that of Susana Puig from Barcelona. She presented the signs of nodular melanoma, a form which is hard to recognise and diagnose. Nodular melanoma accounts for around 15% of melanoma cases. The first clue is that patients often observe a change in the lesion, and that it is more common in older men. Dermoscopy is important – it is often an asymmetrical lesion with no melanocytic network or aggregated globules. We can often see three or more colours (red, blue, black and/or white). The blood vessels are abnormal (hairpin vessels that are atypical, punctiform, tortuous or polymorphic, as well as milky, reddish areas). Unstructured areas, a bluish-grey veil and shiny whitish striae are common. Certain lesions may resemble haemangioma with structures evocative of vascular saccules. It is essential that we do not propose clinical treatment for this type of nodular lesion, but rather an immediate biopsy.
Speakers: Dr. Phyu Aung, Dr. Susan M. Swetter, Dr. Clara N. Curiel-Lewandrowski and Dr. Hensin Tsao
Report summarised by Dr. Joël Claveau
Speaker: Dr. Susan M. Swetter
Report summarised by Dr. Joël Claveau
Speaker: Dr. Clara N. Curiel-Lewandrowski
Report summarised by Dr. Joël Claveau
Speaker: Dr. Hensin Tsao
Report summarised by Dr. Joël Claveau
Report written by Prof. Brigitte Dréno
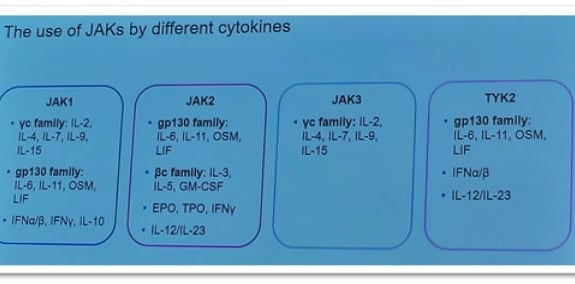
JAKs are enzymes linked to cytokine receptors. Activation of a JAK by a cytokine then leads to activation of a transcription factor called STAT, which in turn activates the genes involved in chronic inflammation. Therefore, JAK inhibitors make it possible to block multiple cytokine production pathways, in contrast to biotherapies which target a specific receptor or cytokine.
The FDA has required a “Warning” on the packaging. These treatments cause nausea, pharyngitis, headaches, and facial folliculitis. More problematically, they are associated with an increase in herpes and shingles infections. The Americans therefore believe that vaccination should be advised before starting this treatment. Before initiating treatment, they also recommend that HIV and hepatitis tests be performed. A dosage of CPKs and lipids is also recommended before starting treatment, at four weeks and three months afterwards.
IL15Rβ induces re-pigmentation by a new mechanism that depletes memory T cells. Studies on the role of Tregs are also in progress.
Other diagnoses to consider, with some new therapeutic solutions:
Report written by Prof. Brigitte Dréno
Pustular psoriasis is associated with the IL-36/IL17c pathway, which controls neutrophil infiltration. Two IL36-R inhibitors are now on the way for generalised pustular psoriasis: spesolimab and imsidolumab.
Report written by Prof. Brigitte Dréno
Your choice of…
Report written by Prof. Brigitte Dréno
Though neglected thus far by our discipline, climate change (and temperature increases in particular), combined with increased pollution, has a very significant impact on our skin.
This impact starts on normal skin, with a modification of the skin microbiome in connection with the increase in skin temperature, followed by modification of our adnexal glands, and culminating in a skin dysbiosis that can favour the appearance or outbreaks of inflammatory skin diseases.
Pollution increases skin pigmentation disorders, e.g. by way of an increase in oxidative stress.
An increase in auto-immune disorders like lupus has also been observed, not only in the skin but in terms of systemic effects including renal involvement.
The frequency of pemphigus and the severity of outbreaks has also increased.
Viral diseases, and herpes in particular, are now more frequent.
Outbreaks of psoriasis, and of atopic dermatitis with more intense pruritus, have also increased in frequency.
Another factor has to do with changes in the geographic distribution of parasitic diseases, illnesses linked to insect bites.
Finally, a positive correlation has been shown between reduction of the ozone layer and development of wrinkles, independently of co-pollutants (PM10 and NO2).
Skin pathologies related to climate changes and the degradation of our environment are becoming a treatment priority and a public health issue of which there is still very little public awareness.
Report written by Prof. Brigitte Dréno
For example, skin health depends on regular physical activity, now defined as 150 minutes per week of moderate physical activity or 75 minutes of intense physical activity. Today, 25.6% of adults report that they don’t have time for physical activity, with a slight predominance among women at 27.9%, vs. 23.1% of men.
Simultaneously, the prevalence of obesity is increasing in every country in the world, with projected figures above 45% in the United States, 35% in England, and 20% in France.
Obesity combined with a lack of physical activity is associated with an increase in chronic inflammatory diseases, infectious skin diseases, and auto-immune pathologies.
Report written by Prof. Brigitte Dréno
If there’s one point that’s essential to remember with regard to skin cancers, it’s the role of the intestinal microbiome in controlling the therapeutic response to PD1 inhibitors. Recent work shows that the intestinal microbiome of immunotherapy non-responders has a bacterial profile different to that of immunotherapy responders. In particular, it appears that treatment with systemic antibiotics in the month prior to the start of immunotherapy is associated with a sharply higher rate of therapeutic failure. Through their secretions, including secretions of certain antimicrobial peptides, the bacteria of the intestinal microbiome are believed to interact with the Treg lymphocyte populations that reside permanently in the intestinal mucosa, ultimately leading to their migration out of the intestine – a phenomenon that induces chronic inflammatory diseases like Crohn’s disease or promotes the development of certain cancers. Against this background, faecal transplantation looks like the therapeutic approach of the future in combination with immunotherapy. Stay tuned...
Advanced forms of inoperable basal cell carcinomas can now benefit from the use of Hedgehog pathway inhibitors. However, this orally-administered drug is associated with side effects than may limit its use, notably muscle cramps. L-carnitine may be able to reduce or even eliminate this side effect.
Hydrochlorothiazide appears to be associated with a higher risk of basal cell or squamous cell carcinomas, and this effect is linked to cumulative use. Having now been described for the first time, we should certainly be looking out for this effect in the future for our patients…
A genetic signature identified from a biopsy of primary tumours may be able to predict the risks of a positive sentinel lymph node biopsy, and thus to limit the use of this procedure. Stay tuned… Of course, this would certainly be a benefit to our patients.
Dear Colleagues,
It is a great pleasure to have been invited by Bioderma to attend the AAD Annual Meeting in Boston and report back to you. The conference began with a buzz in the air as the first face to face world dermatology conference following the pandemic started. My day began by attending the Medical and Surgical Management of Nail Disorders with a great selection of speakers from around the world sharing their experience.
Speakers: Dr. Shari Lipner, Dr. Mark J. Holzberg, Dr. Antonella Tosti, Dr. Bianca Maria Piraccini, Dr. Jane S. Bellet, Dr. Molly A. Hinshaw, Dr. Dimitris Rigopoulos, Dr. Julia O'Brien Baltz, Dr. Nathaniel J. Jellinek and Dr. Chris Adigun
Report written by Dr. Ben Esdaile
The session opened with Shari Lipner from New York talking about how she manages onychomycosis. She talked about the importance of using dermoscopy to aid in the clinical diagnosis but also the importance of confirming the diagnosis before systemic therapy. She mentioned the potential future use of AI as an adjunct in and the role of telemedicine in following up patients for their treatment. Oral terbinafine is still her treatment of choice for healthy adults and she recommended no interval monitoring of bloods for those with no risk factors.
Mark J. Holzberg from Georgia then spoke about managing longitudinal melanonychia. He emphasised the importance of looking at all 20 nails to establish if multiple or single. If there is a suspicious evolving single band you need to exclude melanoma. He advised keeping the biopsy to the distal nail matrix and getting the largest sample as possible.
Antonella Tosti gave her tips about onychotillomania. She highlighted the importance of firstly not missing the diagnosis with helpful clues being the absence of the cuticle and nail plate with crusts and sometimes pigmentation. She showed useful dermoscopic tips including the oblique arrangement of nail bed haemorrhage and wavy lines. She then talked about the possible use of N-acetylcysteine (600mg 3x day) as well as habit reversal to treat it. The session continued with talks from Avner Shemer from Israel talking about both acute and chronic paronychia and highlighting the importance of treating the cause particularly when infection is involved. Adam Rubin from Pennsylvania then gave a talk around the tricky subject of paediatric melanonychia. He reassured us about how exceptionally rare paediatric nail matrix melanoma is but did highlight that cases do exist. He showed cases of melanonychia that spontaneously resolve after a few years. He also highlighted the importance of good histopathology if a biopsy is taken.
Bianca Maria Piraccini from Italy then simplified the management of longitudinal erythronychia breaking it down into single or multiple bands. With single bands you must think about malignancy but with a history of pain and aggravation with the cold, think about glomus tumours. Small hyperkeratotic masses at the distal nail plate are helpful in recognising onychopapillomas.
Jane S. Bellet from North Carolina then gave us some useful tips for paediatric nail disorders. She highlighted the Importance of a soft and slow approach when examining young children. She gave tips on recognising congenital hypertrophy of nail folds and tips in management including soaks, topical steroids and taping. She also talked about recognising lichen striatus of the nail with a conservative approach and patience.
Molly A. Hinshaw from Wisconsin then gave us tips in the management of Glomus tumours and the importance of one surgical procedure aided by good prior localisation with either transillumination, ultrasound or MRI. She then showed us surgical management with partial nail avulsions with blunt excision of the tumours.
The session continued with Dimitris Rigopoulos from Greece giving us advice on the management of nail psoriasis. He highlighted that this should be personalised to the patient depending on numerous factors. He talked about the topical management depending on the number of nails and whether the nail matrix or bed were involved. He mentioned a recent paper showing the successful use of 0.025% tretinoin for 3 months. He also discussed the use of intralesional steroids and methotrexate and then for multiple nails systemics including methotrexate, ciclosporin and acitretin. He then also touched on the use of biologicals and smaller molecules.
We continued with Julia O'Brien Baltz from Massachusetts talking about retronychia with the stacking of the nail plates often in females and dancers. She discussed the principals of treatment in decreasing inflammation and removing foreign body (stacked nail plate).
Nathaniel J. Jellinek from New England then gave a talk on the management on nail melanoma. He highlighted the importance of functional surgery more than amputation.
Clear margins are the most important but digit-sparing surgery, particularly in in-situ cases, has a big impact on quality of life.
We also had two rare interesting cases presented with the first from Chris Adigun from North Carolina showing us an interesting case of Gadolinum deposition disease in a patient with normal renal function exposed to Gadolinium presenting with brittle nails and rubbery swollen digits. The session concluded with April Schachtel from Washington showing a case of nail sarcoidosis with underlying bony cysts.
Speakers: Dr. Jerry Shapiro, Dr. Natasha Atanaskova Mesinkovska, Dr. Sergio Vano-Galvan, Dr. Elise A. Olsen, Dr. Antonella Tosti, Dr. Leonard C. Sperling, Dr. Kristen Irene Lo Sicco and Dr. Azael David Freites Martinez
Report written by Dr. Ben Esdaile
The aim of this session was a general update in hair disorders. The session was chaired and started by Jerry Shapiro from New York who introduced the session with his guide to managing cicatricial alopecias. He described cicatricial alopecias as trichologic emergencies and advised early aggressive treatment. He split the scarring alopecias into lymphocytic, neutrophilic and mixed. He showed the use of dermoscopy to judge activity. In Lupus erythematosus he discussed the use of TCM (individually applied topical Tacrolimus, then topical Corticosteroid and then 5% Minoxodil) as well as the potential use of low dose oral minoxodil. For more extensive disease (>10%) he advised hydroxychloroquine with the consideration of an oral prednisolone bridge. He discussed a similar approach to lichen planopilaris and Pseudopelade of Brocq with more recalcitrant cases he talked about the use of finasteride or dutasteride and then pioglitazone or naltrexone. Finally, he talked about the possible use of Excimer laser as well as some the potential use of baricitinib.
For frontal fibrosing alopecia he divided the management in to rapidly or slowly progressive. For rapidly progressive he suggested oral prednisolone (40mg/d for 1 week then taper by 5mg/week for 8 weeks). For slowly progressive he suggested the TCM combination as well as intralesional steroid injections. He discussed the addition of numerous therapies depending on response including 5-alpha reductase inhibitors (finasteride in premenopausal and dutasteride in postmenopausal), hydroxycholoroquine, doxycycline, low dose oral minoxodil, pioglitzone and naltrexone. He finally also suggested other treatments if not responding including platelet-rich plasma (PRP), excimer laser, mycophenolate, methotrexate and oral retinoids. He did also discuss the possible role of sunscreens in facial moisturisers as a possible trigger and advised against chemical sunscreens avoiding oxybenzone and avobenozone particularly. In the final part of his talk he discussed some novel treatments for other scarring alopecias including topical 10% metformin for central centrifugal cicatricial alopecia (CCCA). He also discussed novel treatments for refractory folliculitis decalvans with adalimumab as well as baricitinib.
In the second part Natasha Atanaskova Mesinkovska from California gave an update in Alopecia Areata. She reminded us of the high prevalence (2% of population) and the fact this is increasing with higher rates in certain populations (e.g. Afro-Caribbean). She discussed the possible role of vaccines and viral infections especially during the recent Covid pandemic. She then discussed novel treatments with JAK inhibitors including Baricitinib, Ruxolitinib and Rofactinib. She highlighted good response rates (46-75%) and the fact they are well tolerated. Long term use is needed as hair loss will occur if stopped. She also reminded us of the black box warnings of serious infections, cardiac events, malignancy and thrombosis. She finished off by discussing the potential role of dupilumab as many alopecia areata patients tend to have raised IGE. She suggested IGE as a good marker and worth considering dupilumab if raised. She finally mentioned Etrsimod (S1P modulator) as a potential treatment in the pipeline.
The next speaker was Sergio Vano-Galvan from Spain who gave us a hair surgery update.
He discussed the importance of the correct indication for hair transplantation and the importance of making sure medical treatment is tried first. He also highlighted that the transplant was not a cure and medical therapy is also needed after transplantation to stop worsening over time. He also showed us his micrograft technique as well as the potential of that use of robotics as an aid in the future.
He was followed by Elise A. Olsen from North Carolina who discusses chronic telogen effluvium with a number of different mechanisms. She explained of the importance of showing global shedding using a gentle hair pull and a dermatoscope to check for telogen hairs. She highlighted the need for a good history and checking bloods including iron, vitamin d, zinc and thyroid function. In terms of management she discussed oral or topical minoxodil and warning patients in regard to the potential of hypertrichosis.
We were then treated to a trichoscopy masterclass by Antonella Tosti from Italy. She showed us the role of dermoscopy in showing hair shaft variability in androgenetic alopecia, broken hairs in alopecia areata and loss of follicular openings in scarring alopecia. She showed the signs of early scarring with peripilar casts, pili torti and a loss of vellus hairs. She also emphasised using dry trichoscopy as contact mediums will oblate the scale signs.
Next Leonard C. Sperling from Baltimore delivered an excellent lecture on aiding the Dermatopathologist in giving accurate meaningful results. He explained that a histology report is an opinion and is dependent on the correct biopsy site. He highlighted the importance of providing the pathologist with the correct information as well as the correct biopsy site. He showed that in non- scarring alopecias the best biopsy site tends to be in the baldest spot. In scarring alopecias, the best spot is a site with early or mild involvement. Dermoscopy can aid in this.
The penultimate talk was from Kristen Irene Lo Sicco from New York about Platelet Rich Plasma (PRP). Kristen gave us useful practical advice and a video for patients to advise no anticoagulants for 1 week prior to PRP. Patients should also avoid alcohol both immediately before and after. She showed the off label use in androgenetic alopecia, alopecia areata and CCCA. The mechanisms are not fully understood but the platelet derived growth factors appear to promote anagen and vascularisation. She also showed analagesia techniques including vibrating devices.
The final talk of the session was by Azael David Freites Martinez from Spain who talked about hair loss in cancer patients and survivors. He talked about chemotherapy induced alopecia (CIA) particularly after the use of taxanes. He discussed the potential role of scalp cooling systems in prevention. He discussed potential side effect of headaches. He then went on to discuss persistent CIA. He talked about potential treatment with topical as well as oral minoxodil and oral sprinolactone. He highlighted not to use finasteride or dutasteride in Breast cancer patients. He then showed images of endocrine therapy induced alopecia (ETIA) particularly in breast cancer patients. Both CIE and PCIE have the similar treatments.
Speakers: Dr. Sandy Tsao and Dr. Shadi Kourosh
Report written by Dr. Ben Esdaile
I started Day 2 of the conference with a session chaired by Sandy Tsao from Boston entitled Fifty Shades of Brown. She highlighted the importance of the changing demographics in the USA with it diverse and multi-ethnic population. She reminded us that skin of colour has the same number of melanocytes but the difference is the melanosomes within the melanocytes. Hyperpigmentation can result from an increase in melanin production or decreased degradation of melanin.
Her first tip was to determine where the pigment is and whether it is epidermal or dermal in location. She uses a Woods lamp which highlights epidermal pigment. She discussed the common conditions she sees including post-inflammatory hyperpigmentation (PIH), melasma, photoageing and periorbital hyperpigmentation (dark circles).
She advised managing patient treatment expectations and discussed several treatment options. She discussed the importance of good sun protection with newer formulations of sunscreens with titanium dioxide and zinc oxide helping also protect against visible light. She suggested the use of cosmetic camouflage to help patients as pigmentary disorders have an enormous impact on patient’s quality of life.
In terms of topicals treatments she discussed the pros and cons of topical hydroquinone (HCQ) but also enthused about azelaic acid as one of her favourite treatment options with its anti-inflammatory as well as tyrosinase inhibitory effects. She suggested the use of topical retinoids to help epidermal skin turnover as well as the possible aid in the absorption of other molecules. She also highlighted other cosmeceutical ingredients including Kojic acid, Bearberry, liquorice extract (more potent inhibitor than HCQ). She interestingly opts for liquorice extract over HCQ. She also suggested some benefit with ascorbic acid – an antioxidant that can weakly inhibit the production of melanin. The caution however is its limited stability and rapid oxidation.
For melasma she discussed topical tranexamic acid (TA) and its difficulty in absorption. It has the benefit of inhibiting keratinocyte transfer, vascular contraction and reducing inflammation. She described some benefits in selected patients of oral TA (500mg daily for 3 months). This can be more helpful for epidermal melasma but there are still concerns with those at risk of thromboembolism.
She went on to show the use of chemical peels (superficial) with alpha and betahydroxy acids with some excellent results. She then showed benefits with microneedling for recalcitrant melasma with the added benefit of helping the absorption of molecules such as TA. She confirmed laser can help but should be used in the correct patients with caution. Laser can also be helpful in other cases of pigmentation including naevus of Ota and café au lait macules. She demonstrated that Pulse dye laser can help in the vascular components of melasma and brought to our attention the potential of oral antihistamines combined with vascular lasers for melasma in the future.
Next Shadi Kourosh, also from Boston, gave her inspirational approach to dyspigmentation.
She highlighted the importance of all dermatologists being aware of diversity in skin colour with people of darker skin types composing more than half the world’s population. She talked about the principals of managing pigmentation in particular some of the more challenging aspects. She discussed that tyrosinase is still the key enzyme target in melanin production but newer targets include the PAR-2 enzyme involved in melanin transfer.
She quoted Confucius in that ‘Nature makes humans the same, life makes them different’.
She discussed the multiple environmental factors including ultraviolet and visible light. She also discussed Infra-red radiation and it role in some types of melasma (e.g. a kitchen worker exposed to heat). Other factors discussed included latitude, altitude, reflection and the ozone. She also highlighted the importance of air pollution and the need for good cleansing regimens for those who live in cities.
She highlighted pillars of therapy for hyperpigmentation:
She discussed the importance of sun protection including against visible light. She gave a tour around topical and oral medications as well as bringing to our attention unsafe skin practices occurring in many parts of the world, including Boston, of skin bleaching products such as glutathione.
Speakers: Dr. Brett Andrew King, Dr. Jeffrey M. Sobell, Dr. David Rosmarin, Dr. Ruth Ann Vleugels, Dr. William Damsky, Dr. Brittany Gareth Craiglow, Dr. Eric Lawrence Simpson, Dr. Matthew Vesely and Dr. Brett Andrew King
Report written by Dr. Ben Esdaile
The aim of this session was an overview of JAK (Janus kinase) inhibitors and their role in dermatology. The session was chaired by Brett Andrew King from Connecticut who started with an overview of the family of JAK inhibitors (JAKi) including JAK 1, 2, 3 and TYK2 and the numerous cytokines that signal through the JAK-STAT pathway.
He was followed by Jeffrey M. Sobell from Boston who talked about JAK inhibitors for psoriasis. He showed us that several key cytokines in psoriasis function through the JAK/STAT pathways. The risk/benefit of the oral agents inhibiting JAK1,2 and/or 3 require further studies. He showed us some potential side effects with JAK 1 inhibition with dose depended increases in cholesterol and lowering of platelets. Some of the studies with JAK1/2 inhibition (baricitinib) also showed some falls in lymphocytes and neutrophils as well as anaemia and rises in creatinine kinase. He showed us that there are some early investigations of topical JAKi including tofacitinib. The most promising oral agents for psoriasis appear to be the sole TYK2 inhibitors (Deucravacitinib). Their phase III efficacy and safety results are encouraging. Their safety profile seems better with side effects of nasopharyngitis and upper respiratory tract infections as well as low rates of folliculitis and acne. The laboratory profiles seem less problematic and the results are promising.
Next David Rosmarin, also from Boston, talked about the use of JAKi in Vitiligo. He discussed the potential use of Tofacitinib (JAK1/3) and Ritlecitinib (JAK3i) with promising clinical trial data. He discussed the benefits of topical JAKi over oral JAKi for vitiligo given the superficial site of pathogenesis. He showed some results from the use of topical tofacitinib for leukotrichia as well as Ruxolitinib cream for face and body vitiligo. Study data appears to show that the process takes time (even after 52 weeks). The JAKi seem to work for patients who have had vitiligo for years. The topicals seem well tolerated with minimal side effects with the main ones being application site acne and mild pruritus. The face seems more responsive and he also discussed the possible addition of phototherapy with both oral and topical agents.
Ruth Ann Vleugels from Boston discussed the use of JAKi in her connective tissue disease clinic in particular for dermatomyositis and lupus. She presented some excellent case studies of refractory dermatomyositis responding well to Tofacitinib 10mg bd (JAK1/3i). She also presented some paediatric cases responding well (5mg bd). She presented some lupus patients with some partial responses to tofacitinib. Data from clinical trials showed no clinical skin improvement for Baricitinib with improvement in joint disease more than skin. She also had some promising results in sclerosing diseases with tofacitinib.
William Damsky from New Haven talked about JAKi in sarcoidosis and granuloma annulare. He showed some excellent responses to tofacitinib both orally and topically in sarcoidosis (both systemic and cutaneous). He shared his data from an open label trial at his hospital of 10 patients with 6/10 having a complete response while the other 4 had partial responses with no serious side effects but emphasised that larger controlled studies are needed. He also showed some promising data and images of his patients with generalised granuloma annulare treated with oral tofacitinib.
Brittany Gareth Craiglow from New Haven then discussed the potential role of JAKi for alopecia areata. Her take home message was that the topical agents don’t really work but the orals do. She summarised that Ruxolitinib cream and delogocitinib ointment appear to be ineffective. She then showed some data from a phase III study published today of oral Baricitinib. This appears to be highly effective with complete or near complete hair regrowth in the majority after 6-9 months. She gives adjuvant oral minoxodil to all and patients appear to need continuous long term treatment.
Eric Lawrence Simpson from Oregon summarised the use of JAKi in atopic dermatitis. In the topical field he showed that early data with topical Ruxolitinib is encouraging. It appears to have similar efficacy to a medium potency topical steroid without significant side effects. The safety data is excellent with minimal absorption. The cost however is still prohibitive.
The oral JAKi fill a gap especially being oral, potent and providing a rapid itch response.
Upadacitinib and abrocitinib (JAK1i) show good responses that appear better than biologics. There was some nausea with abrocitinib as well as some acne and herpes zoster. Early data is encouraging but they are associated with the very low risks of cardiovascular death, venothromboembolism, cancer and serious infections. Patient selection will be important.
Matthew Vesely from Connecticut highlighted the use of JAKi in a number of other inflammatory dermatoses. In Hidradenitis suppurativa he showed some phase 2 data for JAK1 inhibitors showing a reduction of inflammatory nodules with improved patient-reported outcomes. He showed cases of improvement in lichen planus as well a case of DRESS with myocardial involvement that improved with tofacitinib in addition to pulsed methylprednisolone. He also finally showed some promising results with JAKi (tofacitinib) in morphoea, eosinophilic fasciitis and systemic sclerosis.
Brett Andrew King finished the session by summarising the safety and risks of using JAK inhibitors. Commonly reported mild adverse events include URTI, headaches, nasopharyngitis, nausea and acne. Oral and topical agents carry similar black box warnings of serious infections, mortality, malignancies, cardiovascular events and thrombosis. He highlighted however how rare these events appear and were based on studies in rheumatoid arthritis with a population not necessarily the same as some of our dermatology cohort of patients. These agents will need to be used with caution with patients with risk factors.
Speaker: Dr. Martin N. Zaiac
Report written by Dr. Ben Esdaile
This session was run by Martin N. Zaiac from Miami. He started by emphasising the need to identify the location of the lesion whether in the nail matrix, nail bed or nail unit before starting any surgery. He reminded us of the anatomy of the nail unit and explained that the proximal nail matrix grows faster giving the curvature to the nail plate. He also emphasised the parallel ridge and grooves of the nail bed explaining the formation of linear splinter haemorrhages.
His first really useful tip was for dealing with the thick and hard nail plate. He soaks the nail and finger in a combination of antiseptic (chlorhexidine and saline) for 15 minutes prior to surgery to firstly soften the nail plate as well as disinfect the surgical site.
His simple tip for haemostasis was using a surgical glove tourniquet technique. He puts a smaller sterile glove onto the patient’s hand and then cuts off the tip of the glove on the offending finger and rolls it down creating a simple and cheap tourniquet.
He then showed a collection of cases scattered with useful tips. For subungual haematomas he uses an 18G needle to twist and drill through the nail plate to allow blood to release while keeping the nail plate intact. No anaesthesia is usually needed for this procedure. He also showed a simple technique of needle aspiration of myxoid cysts to help prevent damage to the nail matrix.
For tumours of the nail bed he advised to consider getting an X-ray to exclude bony exostoses to avoid surgical surprises and also consider an MRI if a glomus tumour is suspected.
His main tip for anaesthesia was the dilution of lidocaine and adrenaline with saline to allow more volume and less discomfort. He showed his distal nail block technique followed by further injections to the hyponychium and nail matrix.
For all his techniques he reiterated the importance of sparing the nail plate to decrease pain and improve cosmetic results. He showed videos of the way he approaches numerous pathologies including cutting a parallel incision through the nail plate for onychopapilloma and then over sewing with 3/0 Ethilon. He explained that 3mm is the key width to keep under when making excisions through the nail matrix to try and prevent permanent nail dystrophy.
For melanonychia he showed a number of nail plate saving techniques including a Submarine Hatch technique. This involved making a punch incision through the nail plate (making a hatch) and then using a smaller punch to make the biopsy. He then would use ‘crazy glue’ to stick the hatch back down. The glue will need to be reapplied every 2 weeks to keep the nail intact.
He showed us his tangential shave matrix biopsy for larger (>3mm) pigmented bands with the aid of saline to lift the matrix to make the shave easier. He also showed a Trap Door technique again to preserve the nail plate as well as a Lateral Roll technique to expose larger areas of pigment. With the latter technique the nail plate would be sutured back in place.
In the final section he showed the importance of excising nail bed tumours down to periosteum but not forgetting to warn the patients of likely resultant onycholysis in the area.
Speakers: Prof. Aimilios Lallas, Dr. Bengu Nisa Akay, Dr. Ofer Reiter-Agar, Dr. John Paoli and Dr. Konstantinos Liopyris
Report written by Dr. Ben Esdaile
The symposium on Advanced Dermoscopy was delivered by a collection of dermoscopists from around the world.
The current International Dermoscopy Society president, Aimilios Lallas from Greece started the session with an approach for the early recognition of lentigo maligna with his Inverse Approach.
Recognising early lentigo maligna can be extremely challenging as the known dermoscopic criteria of lentigo maligna (including rhomboidal structures, asymmetrical follicular pigmentation, grey dots etc.) present late on in the disease. With the inverse approach the key is to recognise at least one of 6 benign features as the predominant features to recognise the main differentials - either actinic keratoses or solar lentigo (For actinic keratoses - scale, white and wide follicular openings (rosettes) and erythema. For solar lentigo - Parallel lines (fingerprinting) or reticular, sharp demarcation of the border and the presence of classic seborrhoeic features such as milia-like cysts and comedo-like openings). If you see one of these features as the predominant feature then the diagnosis is likely to be benign whereas if none of these features are seen then lentigo maligna should be excluded.
Bengu Nisa Akay from Turkey then discussed dermoscopy on heavily pigmented skin. She highlighted the lack of studies on the dermoscopy of heavily pigmented skin in the literature and how challenging some cases can be. She showed some clues for inflammatory dermatoses from examples in her department including white lines to help recognise lichen planus pigmentosus, follicular plugs in folliculotropic mycosis fungoides as well as facial discoid lupus. She then showed the challenges of identifying tumours in heavily pigmented skin. She showed examples of blue-black structureless areas with follicles in naevi whereas in BCCs the blue structureless areas tend to destroy the hair follicles.
For seborrhoeic keratoses the comedo-like openings can be heavily pigmented and the blue-white veil structures can make the diagnosis challenging. She also showed the challenge of a parallel ridge pattern of pigmentation in benign acral naevi on heavily pigmented skin.
Ofer Reiter-Agar from Israel talked about using dermoscopy to help recognise the main four BCC subtypes of nodular, superficial, infiltrative and morphoeic. He discussed all the features of BCC including the more recently described MAY globules (Multiple aggregated yellow and white globules). He showed the recognition of the subtype of BCC can help in planning appropriate treatment. He presented his data from a large meta-analysis looking at the most predictable features in each subtype. This is summarised below:
Nodular BCC – arborising vessels (75%) and shiny white structures (43%). In the pigmented nodular BCCs the most common feature were large blue-grey ovoid nests (36%).
In Superficial BCCs a shiny white-red background (79%) and short fine telangiectasia (60%) and small erosions (43%). In the Morphoeaform BCCs porcelain white areas (75%), ulceration (58%) and arborising vessles (51%). In infiltrative BCCs common signs were arborising vessels (76%), Shiny white blotches and strands (100%) and ulceration (44%). Finally, he showed the negative pink network seen in Firbroepithelial of Pinkus and mixed features of basisquamous cell carcinomas.
John Paoli from Sweden gave a talk on his tips for teledermoscopy.
His first tip was don’t be afraid and just do it.
His second tip was that with dermoscopy you do get clues as to whether there is any substance to the lesion.
His third tip was to teach referring colleagues how to take high quality images.
His fourth tip was evaluating new applications using teledermoscopy for surgeons, nurses and other colleagues.
He also warned us of a few traps including live images compared to store and forward technologies with images. He did advise to lower your threshold for face to face reviews for atypical melanocytic lesions.
In the final part of the session Konstantinos Liopyris from Greece talked to us about Artificial Intelligence in Dermatological practice. He talked about how AI can potentially be incorporated into clinical practice in the future. He clearly showed us how AI may be able to augment dermatologists in the future and we should not be afraid of it.
Speakers: Dr. Joseph C. Kvedar, Dr. Seemal R. Desai, Dr. Sangeeta Marwaha, Dr. Dennis H. Oh, Dr. Jules Lipoff, Dr. Trilokraj Tejasvi, Dr. George Han, Dr. Cory Simpson, Sarah S. Asch, Dr. Ivy Lee, Dr. Susan Boiko and Dr. Karen Mckoy
Report written by Dr. Ben Esdaile
The symposium was started by Joseph C. Kvedar from Boston who looked at telemedicine past, present and the future. He initially discussed the taxonomy of telehealth between virtual visits in real time and the use of Store-and-Forward technologies. He discussed the pros and cons of Store-and- Forward technologies with the main pro being the efficient use of time but with major cons being incomplete history and poor image quality. He went on to highlight virtual visits having the advantage of being more like a normal consultation with clarity of questions but a major difficulty with the need for high bandwidth. He also discussed the main limitations of teledermatology being the loss of physical touch, image quality, clear visualisation in hair-bearing areas, the challenge of pigmented lesions and not being able to do total body skin examinations.
Next Seemal R. Desai from Texas talked about how he made it through the pandemic being thrown in to using teledermatology almost overnight. Interestingly many dermatologists shut their offices for 4-6 weeks as it became a legal offence to perform medical procedures in Texas that were not deemed as life-threatening emergencies during the peak of the pandemic. His take home message was that he feels teledermatology has enhanced his practice and now 15% of his visits are still conducted via telemedicine with great patient satisfaction.
Sangeeta Marwaha from Kaiser Permanente in California shared their experience working with a large group of dermatologists using many teledermatology pathways with store and forward technology. She showed data from almost 350,000 consults during the pandemic with about a 1/3 needing to come in for a face to face review and the remainder being managed remotely. Poor image quality was around 7-9% when performed in the doctor’s office but around 12% when performed by patients. Now their new normal is 50-50 mix of office and teledermatology consults. Her key takeaway messages were to try and improve photo quality with information and videos for providers and improving outgoing communication with standard responses with patient friendly language and handouts.
Next Dennis H. Oh from San Francisco shared his experience of teledermatology from the US Department of Veterans affairs with over 1,000,000 encounters in the last decade. Their model includes attending a clinic for photographs (clinic based imaging process) and he showed the problems with this model during the pandemic with a fall of 90% during the lockdown. Now 20% of all consults are through teledermatology with good provider and patient satisfaction.
Jules Lipoff from Pennsylvania then spoke about lessons for the future in regard to teledermatology after the pandemic. He shared the AAD position statement with the importance of high quality teledermatology. He did highlight the digital divide in the US with some patients not having the bandwidth for virtual visits.
Trilokraj Tejasvi from Michigan then introduced the new normal of hybrid practice with a combination of telehealth and face to face encounters. This model combines the use of teledermatology with images and virtual consults. He introduced a triage model depending on the problem. For example, in-person scheduling for total body skin evaluation or concerning skin lesions and diffuse rashes. He then suggested the potential of offering patients teledermatology first for some conditions such as acne with images first prior to the virtual consultation. He did suggest that the patient should always have the option of a face to face consultation if they prefer.
George Han from New York talked about designing a future state where teledermatology continues with quality and easy to navigate platforms. He discussed the critical aspect of image quality. He talked about the differences between App-based and Web-based platforms for the future and working with tech companies to improve the experience and essentially taming technology. He also touched on problems with AI for skin of colour due to the inequality of the image banks used.
Cory Simpson from Washington further highlighted the health quality divide with the potential role of telemedicine for improving health disparities in marginalised and underserved groups. This however is dependent on access to technology. There are also patient barriers including digital literacy, language barriers as well as physical or mental disabilities. He talked about trying to build a bridge over this divide including expanding broadband and potential access through other resources such as public libraries, local community health centres and 3-way conferencing for patients with language barriers and those who may benefit from advocates.
Sarah S. Asch from Minnesota gave us some tips for paediatric teledermatology. She highlighted that her patients and parents have grown up in a technology-centred world (digital natives) with her patients having been born from 2004 onwards. She gave some useful tips include headphones for teenagers if you need to ask difficult questions when their parents are present allowing them to give yes and no answers.
Ivy Lee, an AI specialist, educated us on the use of telehealth and Artificial Intelligence (AI). She essential described AI as a combination of data and maths. She introduced the concept of Augmented intelligence to enhance human intelligence. AI has the potential of helping us in clinical decision support, triaging and quality checking. AI needs to be safe and equitable. Techquity and the digital divide may be further widened by leaving certain groups behind.
Susan Boiko from San Diego talked about internet education in paediatric dermatology. She showed her large team of medical students providing great education (Good Skin Knowledge) in areas ranging from acne to sun protection. The programme has important goals of diversity, equity and inclusion.
Karen Mckoy from Boston finished the symposium talking about International teledermatology also showing a huge increase in its use since the pandemic but also highlighted further disparities in the provision of telemedicine particularly in the developing world.

Dear colleagues,
It is a great honour to have the opportunity to attend once more (and this time in person) the Meeting of the American Academy of Dermatology (AAD) 2022 in Boston, MA. In partnership with Naos/Bioderma, I am pleased to share with you the main content of the sessions I attended today. Let´s get started! Good reading!!
Speakers: Dr. Mathew M. Avram, Dr. Frederick C. Beddingfield, Dr. Rebecca L. Fitzgerald, Dr. David E. Fisher, Dr. Andrew F. Alexis, Dr. Steven Q. Wang and Dr. Molly Wanner
Report written by Dr. Ricardo Limongi
In a field often lacking in evidence, this session addressed fact and fiction in cosmetic dermatology. This session covered common recommendations in cosmetic dermatology, including pre and post treatment recommendations. Speakers evaluated the evidence behind these approaches. What is known or unknown? Questions and topics including neuromodulators, fillers, sunscreens, cosmeceuticals, as well as laser and energy-based therapies were reviewed.
The session was opened by Dr. Mathew M. Avram, warning that lasers are never perfect, and that we should avoid a cookbook approach, like memorizing or replicating settings, and that we must take care of non-calibrated devices False concepts regarding laser and energy-based devices were referred, like “Deeper vascular lesions do not respond well to Pulsed Dye Lasers (PDL)”, “tattoos are easily removable by lasers”, “Lasers are most effective with aggressive treatment settings“. In this case sometimes higher densities, not depth are mandatory, like in acne scars. In case of scars in general, increased density does not mean increased efficacy. For scars erythema, lower fluences are most effective. Another myth is that “Lasers do not promote health, just cosmesis”. He showed evidence regarding reduction of actinic keratosis with fractional lasers and clearance of basal cell carcinoma with PDL and 1064nm laser. According to him, the key to successful treatment is close observation, good clinical dermatology skills, and a healthy dose of skepticism.
Dr. Frederick C. Beddingfield was in charge of talking about the myths involving Botulinum toxins. The first one is “Different products yield different results” – according to him, there is no good evidence to say one way or another; however, good results are generally obtained from all approved products.
The second myth is “Diffusion profiles differ between BoNTA formulations” – in this aspect, he highlighted it is impossible to say and it is likely irrelevant in aesthetic applications. The third was related to the clinical importance of the protein load. According to him, it exists just a theoretical concern as immunogenicity is very low in all products.
The fourth: “Neutralizing antibodies are important determinants of treatment failure in aesthetic indications”. According to the literature, most patients with treatment failure are negative for BoNT antibodies.
The fifth: “Reconstitution solution matters” – he does recommend not to shake the vial (aggressive reconstitution led to 42% longer time to paralysis in study mice). He also defends the benefits of preserved saline in pain reduction.
The sixth: “Volume of injection matters” – he believes it is probably not meaningful in aesthetic doses. The seventh: “Post-treatment protocols are well supported by clinical evidence” – he believes they are not very important, although thinks that exercising the muscles after application may be a good idea with low risk.
The third speaker was Dr. Rebecca L. Fitzgerald, talking about 6 filler myths:
Dr. David E. Fisher remembered that carcinogenic activity of pheomelanin synthesis is amplified by UV, but why lower phototypes (I and II) have fewer nevi when compared to phototype III? A hypothesis could be that red hair background has “invisible” nevi containing pheomelanin not eumelanin. Another condition related to pheomelanin, and risk of melanoma is related to Parkinson´s disease, due to the L-Dopa they take and the higher level of pheomelanin they produce. UVA + pheomelanin = higher risk of melanoma, so the importance of UVA block (potential value of antioxidant activity).
Dr. Andrew F. Alexis began saying that photoaging is not a concern in Fitzpatrick skin types IV-VI as it looks less severe, delayed by one or two decades. In fact, there is a pattern difference compared photoaging in lower phototypes: The first signs are pigment alterations, textural irregularities, benign facial neoplasms, intrinsic structural changes… much more than the fine lines and wrinkles we find in lower phototypes. Another myth is that laser resurfacing is contraindicated in Fitzpatrick skin types IV-
VI. His recommendation is to use lower treatment levels and prophylactic use of hydroquinone (pre and post) to minimize post inflammatory hyperpigmentation (PIH). PIH can be managed in acne scars treatments, like subcision, TCA, radiofrequency, micro needling, picosecond laser, etc. According to him, Phototyping system is not an accurate predictor of PIH. The palmar creases pigmentation scale may be more accurate. The most important is to now the patient: ancestry, response to sun, to injury or inflammation and history ok keloid and hypertrophic scars.
Dr. Steven Q. Wang talked about systemic absorption of sunscreens. In literature, we find that systemic absorption exceeds the threshold levels. Although studies consider an amount of sunscreen unrealistic. Furthermore, it does not imply toxicity or harms. According to the FDA, they are safe and the use of sunscreens in millions of people during decades is also a strong record of safety profile.
Regarding the controversy of Oxybenzone and coral reef toxicity, he pointed several limitations of the studies, like the difficulty to keep corals alive in lab conditions, the poor solubility of Oxybenzone in water. In fact, the situation in coral reefs may be related to the warming of the ocean water.
Last, but not least, Dr. Molly Wanner talked about the effects of blue light exposition (hyperpigmentation, ROS, damage keratinocytes and fibroblasts), as claims related to the protection of blue light increased 170%. Studies show that sunlight exposure is far more important than screens (1-2 hours = 2 weeks. She concluded recommending blue light protection for patients with melasma, PIH and after laser procedures with tinted sunscreens with iron oxide and large particle size.
Speakers: Dr. Richard L. Gallo, Dr. Julie Claire Harper, Dr. Andrew F. Alexis, Dr. David M. Ozog, Dr. John S. Barbieri, Dr. Hilary E. Baldwin, Dr. Emmy M. Graber and Dr. Seemal R. Desai
Report written by Dr. Ricardo Limongi
This session provided an update on state of the art treatment for acne and rosacea. Speakers compared current treatment options for acne and rosacea, and examined information for best practices in use of isotretinoin, hormonal therapy and antibiotics.
Dr. Richard L. Gallo reviewed the pathogenesis o acne, followed by Dr. Linda F. Stein Gold, talking about new drugs, like the combination of 0.1% microencapsulated tretinoin + 3% microencapsulated benzoyl (the encapsulating process allowed the compatibility of the components), the combination of 1.2% clindamycin phosphate + 3.1% benzoyl peroxide and 0.15% Adapalene, showed how long benzoyl peroxide wash should stay on, for example, 5 or 10% - 30 seconds, 2,5% - 15 minutes! She reinforced the topical retinoids act normalizing follicular hyperproliferation, reduce inflammation, decrease C. acnes, but do not reduce sebum. It is a role or the Clascoterone, which competes with DHT for binding to the androgen receptor.
Dr. Julie Claire Harper showed a practical approach to the use of Spironolactone. She prefers the doses of 100mg, concomitant use of oral contraceptives. Higher doses = higher rates of side effects. No need to check K+ in healthy women between 18 and 45, no evidence of increased risk of breast cancer, it takes 3 months to “kick in”, likely long-term treatment, usually in combination with topicals.
Dr. Andrew F. Alexis talked about treating acne in sin of color, showing good results, almost clearing PIH. He defended the use of Azelaic Acid for skin of color.
Dr. David M. Ozog brought tips for treating acne sequalae. In the pathophysiology of acne scarring, he highlighted that lesions have B-cell infiltrate and that inflammation leads to irreversible sebaceous gland destruction. The main scar types are boxcar, rolling, icepick and macular. Treatment can occur during isotretinoin therapy (except mechanical dermabrasion and fully ablative devices). Topicals as Tazarotene can modify scars. Ablative fractional lasers offer best compromise between efficacy and adverse events. Micro needling gets close, and it is now the most common treatment for acne scarring, it is especially effective when associated with other modalities. CROSS technique with TCA 100% using a BD needled syringe is the best alternative for icepick scars. Minimum 2 sessions.
Rolling scars are easier to treat (subcision, micro needling, fillers). Red light PDT and pulsed dye laser are good modalities to treat macular/erythematous scars.
Dr. John S. Barbieri, talking about Isotretinoin monitoring and management of side effects, brought wonderful tips in management of mucocutaneous side effects: use of Omega-3 1g daily, with increase in symptoms of dry lips, dry nose, and dry skin. Besides, the use of antihistamines (Levocetirizine 5mg/day) associated with the Isotretinoin, brought lower incidence of initial flaring. He did not mention the mechanisms involved. Concerning the monitoring tests, he is convinced that we over-test the isotretinoin patients.
Dr. Hilary E. Baldwin, showing what´s new in the treatment of rosacea, talked about BPO micro capsulated (much less irritative) and low dose extended-release minocycline, as well as Serecycline, a tetracycline class antibiotic approved or moderate-severe acne that seems to work well in rosacea. Regarding Mask-Ne and Mask-Acea, she pointed out the factors possibly involved in their genesis, like increasing of temperature, increasing of sebum, disruption of barrier function, dysbiosis.
Sometimes contact dermatitis in the area of the mas can be wrongly diagnosed as rosacea.
According to Dr. Emmy M. Graber, lasers (KTP, PDL, Infrared, CO2) and lights (IPL, LED, radiofrequency and blue light devices) all need better quality studies to evaluate their efficacy. Regarding the PDT, it looks effective, but temporary in treatment of acne. Recently, 1064 laser (FDA approved) may be associated with good results treat acne. The same for two devices with 1726 wavelength (none yet FDA approved). According to him, IPL is safe during the Isotretinoin treatment. In his hands, PDL looks more effective than IPL for treating erythema. Finally, three pearls:
Dr. Seemal R. Desai talked about the pathogenesis of PIH, including inflammatory mediators (PGE2), leukotriens (LTC4 and LTD4), both stimulating melanocytes and in turn, a disruption in the skin´s basal layer. Treatment options include topical retinoids, Azelaic Acid, Hydro quinone, Chemical Peels, Cosmeceuticals, reassurance, and time. Tazarotene looks more effective than Adapalene. He suggests preparing the skin (pre-post peelings) with 4% hydroquinone and to discontinue topical retinoids 7 days prior to the peel. His recommendation is a sequence o 5-6 peels q2-3 weeks. For oral tranexamic acid, best doses seem to be 250-500mg daily. Cysteamine physiologically delivers powerful antioxidant activity in the skin with multiple effects of the melanogenesis pathways.
Speakers: Dr. Adela Rambi G. Cardones and Dr. Kevin C. Wang
Report written by Dr. Ricardo Limongi
In this session, Drs. Adela Rambi G. Cardones and Dr. Kevin C. Wang highlighted articles from the past year that are relevant to the clinical dermatologist.
They focused on basic science articles as well as articles published in non-Dermatology based journals that are likely to impact dermatological clinical care:
That was a resume of what I had the opportunity to attend in the first day of the AAD Meeting in Boston, a congress with a very dense program, extraordinarily rich in content and information. I hope you enjoyed the summary and look forward to being in your company tomorrow again. See you!

That was a resume of what I had the opportunity to attend in the first day of the AAD Meeting in Boston, a congress with a very dense program, extraordinarily rich in content and information. I hope you enjoyed the summary and look forward to being in your company tomorrow again. See you!

Dear all,
The second and busiest day of the AAD Meeting 2022 was really exciting, and here I am, in partnership with Naos/Bioderma, to bring you in avant-première, some of the most interesting information learned during the day.
Speakers: Dr. Pearl E. Grimes, Dr. Lawrence F. Eichenfield, Dr. Darrell S. Rigel, Dr. Susan H. Weinkle, Dr. Seemal R. Desai, Dr. Jerry Shapiro and Dr. Mark Lebwohl
Report written by Dr. Ricardo Limongi
This session reviewed new and emerging therapeutics for patients with psoriasis, melanoma, actinic keratoses, acne, rosacea, dyspigmentation, hair diseases, nail disorders, and non-melanoma skin cancer. The newest and what's hot in dermatology ranging from medical to cosmetic to surgical dermatology were addressed, and in one 3-hour session, virtually the entire spectrum of dermatology was covered.
Regarding the theme “What´s new for hyperpigmentation”, Dr. Pearl E. Grimes focused on quality o life goal. Therapeutic interventions are based on photoprotection (visible, ultraviolet and infrared light), lighteners (triple combination most effective, antioxidants (Polypodium Leucotomus 480mg, Glutathione 250-500mg, Vitamin E 400-800U, Niacinamide 500mg, pycnogenol 5mg, grape seed extract and silymarin), exfoliants, moisturizers, anti-angiogenesis agents (H1 and H2 antihistamines, tranexamic acid), procedures (chemical peels, microdermabrasion, microneedling, PRP, lasers, IPL) and emerging therapies (LYT2, discoloration defense, Multi-action skin tone correcting cream, 4-n Butylresorcinol, Methimazole, Cystheamine, Silymarin, Thiamidol, Tranexamic acid).
Dr. Lawrence F. Eichenfield talked about “What´s new in Pediatric Dermatology therapeutics”, showing new topical agents for pediatric eczema (Ruxolitinib – JAC 1,2 inhibitor, Tapinarof – aryl hydrocarbon receptor agent and Roflumilast – PDE-4 inhibi) and new systemic therapies (Dupilumab, Oral Jak 1), and some other agents in study. For targeted therapy for pediatric psoriasis, there are four FDA approved agents: Ixekimumab, Secukimumab Ustekimumab and Etanercept. There are lots of other agents in study. Other therapeutic updates were regarding molluscum: Cantharidin 0,7% device – excellent data, and topical nitric oxide application. Targeted therapy with Apelisib for port- wine stain with overgrowth associated with PIK3CA mutations/PROS and a new scabicide: Spinosad topical suspension 0,9%.
Regarding skin cancer therapies, Dr. Darrell S. Rigel showed a phase II study o topical Remetinostat gel in patients with BCC, that seems to be effective and well tolerated. According to him, lower awareness of risk among racial minorities leads to melanoma diagnostic delay. He presented the main targeted therapies for melanoma pathways, in groups of targeted antitumor therapy (BRAF – Vemurafenib, Dabraefnib, and MEK – Trametinib and Cobimetinib) and immune checkpoint blockade (CTLA-4 – Ipilimumab, and PD-1 (Nivolumab, Pembrolizumab, Atezolizumab).
For Susan H. Weinkle, the great evolution of the aesthetic dermatology is based on the better understanding of beauty and aging process, increased choices o products, procedures and injection techniques. Soft tissue augmentation changed from treating lines to facial contouring. As an innovation in fillers, she highlighted RHA range from Teoxane – Geneva, with a new rheology concept. She warned about being proud when using fillers off-label. She proposes a combination therapy for facial contouring based on Deoxycholic acid for jowls, HA for cheeks and botulinum toxin for chin and DAO. For her, at the end o the day you should remember that just because you can does not mean you should, less is better, patients are afraid of lips overdone and frozen face. They want to loo natural.
According to Dr. Seemal R. Desai, 2022 is the year o Vitiligo. He has a personal experience with the vitiligo in his family and considers it is a devastating condition, specially within his Indian origin. Sound bytes!
Dr. Jerry Shapiro, presenting “Hair disorders and hair growth”, answered 5 questions:
Dr. Mark Lebwohl showed good data for targeted therapies in psoriasis, including Tapinarof, Deucravacitinib, Apremilast, Bimekizumab, Soneloinab, Upadacitinib, Bariritinib and IL-23 blockers.
Dr. Theodore Rosen brough information about new anti-infectives, including Ozenoxacin (topical non-fluorinated quinolone), non-inferior to retamapulin, Omadacycline (spectacular for cats and dogs bites), aminomethylcycline with uncommon resistance, Cabotegravir, more effective and convenient than oral (two injection, one month apart; then Q2 months), Cantharidin 0,7% device, Abametapir as single-application anti-lice agent, Oteseconazole, with imidazole and triazole-like properties, Tecovirimat for smallpox, Ebanga and Inmazeb for Ebola.
Speakers: Dr. Jerry Shapiro, Dr. Eric Lawrence Simpson, Dr. Murad Alam, Dr. Kelly M. Cordoro, Dr. David Eric Cohen, Dr. Arielle Rachel Nagler, Dr. Kenneth B. Gordona and Dr. Joseph F. Merola
Report written by Dr. Ricardo Limongi
The symposium addressed those "hot topics" established by registrant consensus, a true reflection of member concerns and interests. The session was a "potpourri" of medical/surgical topics, including some with social and economic import. Expert speakers provided "state of the art" material, highlighting recent trends and developments and accenting emerging and innovative therapies. Presentations were derm relevant, clinically germane, and directly applicable to patient care.
Dr. Jerry Shapiro, presenting “Hair disorders and hair growth”, answered 5 questions:
Dr. Eric Lawrence Simpson, regarding Atopic dermatitis, thinks we must consider treating early AD aggressively using appropriate proactive therapy, steroid withdrawal and other diagnoses for new- onset or worsening “red face”, topical Ruxolitinib is a new potent non-steroidal option that fill an important therapeutic gap. Traloimumab is a new safe therapeutic option, inhibitors are potent therapies for biologic failures.
Dr. Murad Alam highlighted interesting new noninvasive lipolysis device, a robotic no-contact 1064 diode, with no bruising or pain in a recent clinical trial, but with FDA approval for abdominal fat only. Injectable cold slurry for lipolysis is targeted to subcutaneous fat and based on suspension o small ice particles in carrier fluid.
Dr. Kelly M. Cordoro brought a potpourri of practical pediatric pearls. She warned in Pediatric Dermatology, many times the risk of undertreatment is higher than the risk of intervention. She encouraged the use of oral minoxidil (1,25-5mg/d) and spironolactone for AGA in adolescent females. N-acetylcysteine (NAC) modifies glutamate levels in brain and is indicated for excoriation disorder (600-2400mg/d). Regarding psoriasis treatment, she recommends individualizing treatment (including evaluating family preferences) and to rethink sometimes the therapeutic ladder (topicals -> phototherapy -> Systemics -> biologics). She also warned that worrisome signs in adults are common in benign pediatric nevi, presenting as longitudinal melanonychia. We should be more conservative.
Dr. David Eric Cohen showed the hot topics in Contact Dermatitis. According to him, nickel is the most important allergen in tests, if we consider by group of allergens, fragrance is the most important. According to him, pathogenesis is not the same across allergen groups. Sensitization is hapten, host, concentration, and surface area dependent. Individuals wearing piercing have significantly more nickel sensitivity in patch tests. Higher number of piercings, higher sensitivity. Patients should submit their own metals in contact tests. Aluminum is the allergen of the year, probably related to the COVID vaccines.
Dr. Arielle Rachel Nagler showed the hot topics in acne. She described the pathogenesis of Maskne, involving humid microclimate, bacterial load, friction leading to chronic follicular inflammation. She suggests antibacterial gentle cleansers and hydrogel with retinoid/antibiotic. Mata-analysis showed no increase in risk of cancer in general within the spironolactone use. Monitoring of K+ is not necessary in healthy adults. No association between psychiatric disturbances and Isotretinoin is found. In fact, suicidal behavior is significantly higher in the year after isotretinoin, reasons are still unknown.
Metformin enhances peripheral tissue sensitivity to insulin, thus reducing IGF-1 and androgenic hormones. Clascoterone 1% cream is a novel topical androgen receptor inhibitor, competes with androgens, specifically DHT, for binding to the androgen receptor. Decreases sebum production and activation of inflammatory pathways. Topical Minocycline 4% foam – lower bacterial resistance.
Trifatotene 0,005% cream targets retinoic acid receptor (RAR) gamma, the most common RAR in the skin. Melanocortin-receptor antagonists are being studied. They potentially decrease sebum production and the gland size. Nitric oxide inhibits C. acnes through oxidative mechanisms and its metabolites and is being studied, as well as synthetic cannabinoid, with anti-sebum, anti-microbial and anti-inflammatory properties.
Dr. Kenneth B. Gordon highlighted what is really new in Psoriasis. For topicals, highlighted Roflumilast (blockade PDE-4 increases c-AMP -> anti-inflammatory mediators) and Tapinarof (binds aryl hydrate receptor -> anti-inflammatory pathways). He is excited to have these topicals soon. For systemics, Bimekizumab (monoclonal IgG1 antibody that binds both isoforms of IL-17) has the most impressive data of any agent. Deucravacitinib is a TyK2 specific inhibitor that does not impact the other JAK pathways from the perspective of safety.
Dr. Joseph F. Merola, talking about Connective Tissue Disease, warned that majority of DLE patients going on to develop SLE did so <1-2 years from time DLE diagnosis. The median time to progression is 453 days, with the first quartile progressing by 303 days. Management of cutaneous LE involves: photoprotection, smoking cessation, consider vitamin D supplementation, consider the presence of SLE. 1st line therapy: antimalarials, 2nd line: MTX, MMF, dapsone, acitretin, 3rd line: Thalidomide, Lenalidomide, biologics (Belimumab, others). Consider hydroxychloroquine blood level testing in refractory cutaneous LE. Emergent therapies: BDCA2 inhibitor, Anifrolumab, Cereblon inhibitors, JAK/TYK. Botulinum toxin in the hands is a therapeutic option for Reynaud Syndrome. Algorithm for dermatomyositis involves strict photoprotection, MTX, MMF and IVIg. Emergent therapies: Tofacitinib, Ruxolitinib, TYK2 inhibitors.
Speakers: Dr. Cheri Frey, Dr. Imara-Safi Scott and Dr. Kavita Mariwalla
Report written by Dr. Ricardo Limongi
Melasma is a constant challenge in skin of color. The session aimed to diagnose, investigate, and formulate a successful management strategy for these patients. Emphasis on newer topical actives for the treatment of pigmentation in skin of color, the use of chemical peels and micro needling and laser and energy-based devices for this challenging skin condition were also covered.
Dr. Cheri Frey called the attention to differential diagnosis from melasma: Riehl melanosis, drug- induced hyperpigmentation, lichen planus pigmentosus, acanthosis nigricans, exogenous ochronosis. Dermatoscopy may help diagnosing ochronosis – blue globules. She strongly encourages dermatologists to use procedures (chemical peels, micro needling, radiofrequency, lasers – low fluence Q-switched Nd:YAG and 650-microsecond 1064nm Nd:YAG short pulse duration).
Dr. Imara-Safi Scott presented a review in Tranexamic Acid (TA). TA is a plasmin inhibitor that prevents binding of plasminogen to keratinocytes -> decrease prostaglandin production -> decrease tyrosinase activity. It also decreases angiogenesis and VEGF expression by decreasing mast cell activity. There is some evidence showing efficacy of topical TA. More evidence is needed. There is stronger evidence showing efficacy for oral TA.
Dr. Kavita Mariwalla showed the best actives in OTCs for melasma, including Niacinamide, Tranexamic Acid, Hydroquinone, Vitamin C, Bakuchiol, Cysteamine, Azelaic acid, Mandelic acid, tretinoin.

This is a summary of what happened today during the AAD Meeting 2022 in Boston. I hope you liked it!
Speakers: Dr. Rodrigo Pirmez, Dr. Jerry Shapiro, Dr. Melissa Piliang, Dr. Maryanne Makredes Senna, Dr. Yolanda M. Lenzy, Dr. Meena Kuimari Singh and Dr. Lynne J. Goldberg
Report written by Dr. Ricardo Limongi
This session presented a practical approach to hair disorders focused on the key differential and therapy. Attendees were updated on how to evaluate scarring alopecia, nonscarring alopecia and how to treat scarring alopecia.
Dr. Rodrigo Pirmez focused on the key aspects of Trichoscopy of non-scarring hair loss. For AGA, miniaturization (>20%) is the best marker. The diameter diversity is related to severity. Comparison between frontal and occipital may help. Single hair units, yellow dots (follicles with no shafts) are also present. In ATE, presence of short regrowing hair. Pseudomoniletrix, broken hairs, black dots (broken close to skin), exclamation mark hair are characteristics of AA. Thin hairs are sign of activity, not regrowth. Short regrowing hair and pig tail regrowing hair are regrowth signs. Yellow dots are related to prolonged telogen. Trichotillomania shows broken hairs of different lengths, with patches never 100% hairless. The trichoscopy in tineas allows initial diagnosis to start the treatment before culture results are available. Corkscrew, comma, Morse code, zigzag hairs, white bands are typical.
Corkscrew, comma suggest Tricophyton and use of Terbinafine, and Morse code, zigzag hairs suggest Microsporum and use of Griseofulvine or Itraconazole.
Dr. Jerry Shapiro explained how he manages TE, AGA and AA. First investigation involves making the patient say “My hair was normal until…”. The main lab tests are TSH, ferritin, zinc, vitamin D, free and total testosterone, DHEAS, prolactin, FAN, Complement, CBC. Triggers for TE are medications, Stress, nutritional, Endocrinologic and autoimmune disorders. Natural story includes 3-6 months of shedding, regrowth in 12-18 months. Treatment of female AGA involves topical Minoxidil as first-line treatment, in combination with spironolactone /dutasteride when monotherapy fails, low dose Minoxidil can be added (0,625-2,5mg/d). Other options are bicalutamide (25-50mg), PRP, prostaglandin analogs, hair pieces and hair transplantation. In his experience, micro needling is not effective.
Measure of hair can be made usually 12cm from glabella to hair line, in case of temporal or vertex thinning, 10cm from outer canthi and 24cm from glabella, respectively. For AA, first line of treatment are intralesional corticosteroids. He suggests low concentrations with higher volumes (9cc per 90 injections, 2.5mgcc). Short courses (6 weeks) of oral corticosteroids stimulate hair growth, Methotrexate is alternative. JAK inhibitors are game changers for AA. Tofacitinib, Ruxolitinib, Baracitinib.
Dr. Melissa Piliang explained that history of scarring alopecias must include nutritional data, symptoms, curse and prior treatments. Lab tests include general health evaluations, nutritional and hormonal (There is association between scarring alopecia and thyroid disease). Others if indicated. Dermoscopy and Wood´s light may help diagnosis. Biopsies must be performed in peripheral areas of the patches. FFA is preferent found in post-menopausal women, affects eyebrow in 50-75% of the cases, less frequent eyelashes. Body vellus involvement. Clinical clues are hypopigmentation, prominent veins, loss o eyebrows/eyelashes, density gradient. Unusual presentations: men, young women, parietal scalp/ophiasis. Beware of lichenoid keratosis.
Dr. Maryanne Makredes Senna brought the “Pearls in the management of scarring alopecia”. Regarding LPP, FFA, CCCA, the first step of the ladder involves avoidance of potential harmful ingredients in personal care, topical metformin 10% (CCCA), topical anti-inflammatory or tacrolimus, intralesional corticosteroid injections every 3 months (maximum 0.25-0.5mg every centimeter.
Second step includes hydroxychloroquine, phototherapy, Dutasteride, Naltrexone (3mg/d), cetirizine/fexofenadine, Gabapentin. Third step: oral JAK inhibitor. Rates of relevant positive tests are higher than those reported in general population. Sunscreens and moisturizers are associated to likelihood of FFA. Very important to remember the hydroxychloroquine-associated retinopathy risk increases nearly fivefold in Tamoxifen use.
Regarding FD, first step involves fluocinonide or Clobetasol 2-3 times//week, BPO wash, Doxycycline 100mg BID or Cephalexin 500mg BID. Intralesional scalp steroid injections every 3 months.
Second step involves oral prednisone or oral isotretinoin (1mg/kg/d 8-10 months, then 10mg/day 6 months). Third step involves Dapsone 75-100mg, Adalimumab or Infliximab.
Dr. Yolanda M. Lenzy showed Styling tricks and helpful tips for ethnic hair loss. She warned ethnic hair requires always gentle hair care, for example, use of therapeutical shampoos maximum 1-2 times per week. Caution with use of “Protective style”. Although they protect from manipulation, increase risk of TA and CCCA exacerbation. Importance of style rotation. Styles: box braids, crochet styling, traditional or sister locs, cornrows, flat twist up-do, two-strand twist-out. She recommends wash & go treatment (involves shampoo and condition, detangle, aloe or flaxseed gel, dryer, curly cut and sleep with satin cap).
Dr. Meena Kuimari Singh advantages and disadvantages of Follicular Unit Extraction (FUE). Among advantages, no linear scar, patients with limited donor tissue, keloid-prone patients, transection rate of follicles can be equal to a donor ellipse. Among disadvantages, the need to trim a wider area (may be an issue for women, time consuming and cost.
According to Dr. Lynne J. Goldberg, hair loss evaluations are difficult, biopsies are often helpful, but sometimes there is poor clinicopathologic correlation. Giving clinical information, indicating, for example, the biopsy was made at the edge of the lesion can help accuracy of the analysis.
Speakers: Dr. Steven Shama and Dr. Hillary Baldwin
Report written by Dr. Ricardo Limongi
The key to effective presentations is feeling passionate about the topic and conveying that passion to the audience in a clear, succinct, and entertaining fashion. Techniques discussed could help attendees to identify their passions, put aside their nervousness, prepare a memorable presentation that is tailored to the specific audience, deliver it flawlessly and eagerly anticipate their next "performance".
According to Dr. Steven Shama, public speaking is one of the most common fears, prior than heights, death, or insects. The aim of his presentation was to try to transform avoiders in resistors, resistors in acceptors, and acceptors in seekers. His four secrets are:
Dr. Hillary Baldwin brought some extra tips: if you want joe telling, you had better be good at it, take care with gestures like gripping the lectern, firing squad, hands in pocket, give emphasis (changing pace, pausing and volume), phrasing of key points. Slides or no slides? Yes, slides, not in excess, use cartoons in spite of photos of dogs or kids.
Speakers: Dr. Darrell S. Rigel and Dr. Steven Q. Wang
Report written by Dr. Ricardo Limongi
Current understanding and novel innovations in photoprotection were discussed by leading experts in the field. The session helped to debunk common misconceptions and controversies about sunscreen. It also shed new insights on photoprotection of the future, highlighting both the challenges and opportunities in view of the changing regulatory landscape by the FDA.
Drs. Darrell S. Rigel and Steven Q. Wang talked about systemic absorption of sunscreens. In literature, we find that systemic absorption exceeds the threshold levels. Although studies consider an amount of sunscreen unrealistic. Furthermore, it does not imply toxicity or harms. According to the FDA, they are safe and the use of sunscreens in millions of people during decades is also a strong record of safety profile. Regarding the controversy of Oxybenzone and coral reef toxicity, he pointed several limitations of the studies, like the difficulty to keep corals alive in lab conditions, the poor solubility of Oxybenzone in water. In fact, the situation in coral reefs may be related to the warming of the ocean water. According to Dr. Darrell, photoprotection beyond UV involves tinted sunscreens, antioxidants: Niacinamide, Licochalcone A, Carotenoids, Vitamins E and C, Glycyrrhetinic acid, DESM, and new filters covering UVA1 (TriAsorB) and visible light. Oral agents are helpful: green tea, Pomegranate, Resveratrol, Curcumin, Silymarin. Complete photoprotection includes shade, clothing, hat, sunglasses, sunscreens.

It was a privilege to participate this AAD Meeting 2022 and, in partnership with Naos/Bioderma, to share everything I have learned with colleagues worldwide. I hope you learned, too. Keep safe and see you the next event!
Speaker: Prof. Henry W. Lim
Report written by Dr. Rémi Maghia
At the “Where do we stand? The Pathogenesis and Treatment of Melasma” session, I chose to focus on the communication of Henry W. Lim (Detroit, Michigan) on photoprotection strategies.
What are the differences between fair and pigmented skin? Phototypes IV to VI have larger melanocytes that contain more melanin. Melanin in skin of colour can filter two to five times more UV rays than melanin in fair skin.
Approximately 5% of UV rays and 50% of visible light (VL) rays reach the Earth’s surface at sea level. Over half of all the free radicals generated by the sun come from the visible light spectrum.
UVB, UVA2: erythema, photocarcinogenesis: especially for phototypes I to III
UVA1: tanning, photo-ageing, photocarcinogenesis: especially for phototypes IV to VI Visible light:
The speaker reviewed the work of Thierry Passeron’s team on the role, in the VL spectrum, of blue light associated with opsin-3, which is the key sensor in the melanocytes of subjects with pigmented skin.
VL + UVA1 induce erythema in fair-skinned individuals and can generate post-inflammatory hyperpigmentation and melasma in subjects with pigmented skin.
The available organic (chemical) filters are not sufficient to protect against VL.
1/ Tinted sunscreens (SPF 30+, broad spectrum)
The article by Lyons, JAAD May 2021, reviewed photoprotection beyond UVs for tinted sunscreens. Chemical formulations include red, yellow and black iron oxides and titanium dioxide, with different absorption profiles.
The article by Torres, JAAD December 2021, provides a practice guide to tinted sunscreens; it is available online at the following address: http://dx.doi.org/10.17632/dtb4y9b684
It is specified that there are no specific guidelines for tinted sunscreens, aside from “broad spectrum” and SPF appearing on the label. The article lists 53 SPF 30 or higher tinted sunscreens containing iron oxide that are classified by average price per ounce; the list includes the products of certain French brands.
2/ Sunscreens with biologically active antioxidants
Topical antioxidants and VL + UVA1: the article by Lyons, Photochem. Photobiol. 2021 in press compared an antioxidant 2% vs control. For phototypes I to III: decrease in erythema; for phototypes IV to VI: reduced immediate pigment darkening (IPD) and delayed tanning.
The antioxidants contained in sunscreens can be: niacinamide, licochalcone A, carotenoids, vitamin C, glycyrrhetinic acid, DESM.
3/ Sunscreens with new filters covering UVA1 + VL
These include MCE whose filter is Mexoryl 400, and TriAsorb.
4/ Oral adjuvant photoprotection agents
Polypodium leucotomos extract (PLE): study by Mohammed, December 2019, concerning 22 phototype IV to VI subjects, PLE twice daily for 28 days + VL: significant difference in pre- and post- PLE pigment levels.
Another study in Singapore in 2018 compared, for three months in Asian subjects with melasma, the effects of a placebo + hydroquinone 4% + SPF50+ sunscreen vs PLE + hydroquinone 4% + SPF50+ sunscreen, with a significant difference in Melasma Area and Severity Index (MASI) scores.
In conclusion, photoprotection strategies for melasma include: Tinted sunscreens
Sunscreens with biologically active antioxidants Sunscreens with new filters covering UVA1 + VL Oral adjuvant photoprotection agents
Speaker: Dr. Diane M. Thiboutot
Report written by Dr. Rémi Maghia
During the “Acne guidelines” session, Diane M. Thiboutot (Hershey, Pennsylvania) reviewed the long-standing issue of using antibiotics (ABs) for shorter or longer periods in acne.
Benzoyl peroxide (BP), and BP combined with erythromycin or clindamycin, are effective acne treatments; they are recommended as monotherapy for cases of mild acne. BP is effective for the prevention of bacterial resistance.
Topical antibiotics (erythromycin, clindamycin) are effective treatments but are not recommended as monotherapy due to the risk of bacterial resistance. Topical minocycline was approved by the FDA in 2019.
They are recommended for cases of moderate to severe inflammatory acne resisting topical treatments.
Doxycycline and minocycline are equally effective.
Oral erythromycin and azithromycin can be effective against acne; they should only be used by patients who cannot use cyclines (pregnant women, children under the age of 8). With erythromycin, there is also an increased risk of bacterial resistance.
Monotherapy with a systemic antibiotic is not recommended. Trimethoprim-sulfamethoxazole should only be used by patients who do not tolerate cyclines and in cases of resistance to treatment.
The duration of use should be as short as possible: re-evaluate after three or four months to minimise resistance. Concomitant topical BP or a topical retinoid should be used and then continued as maintenance treatment following systemic antibiotic therapy.
In 2015, the WHO reported the global emergence of AB-resistant bacterial strains. There is epidemiological evidence of AB use being associated with upper airway infections, pharyngitis, IBD, and breast cancer.
The emergence of resistant bacteria can concern the commensal flora and the temporarily pathogenic flora, including Staphylococcus aureus and Streptococcus pyogenes.
A pilot study (Chen, JAMA Dermatol 2019) showed that the microbiome changed with four weeks of oral treatment with minocycline: a significant decrease in Cutibacterium acnes was found with a significant increase in Pseudomonas. Eight weeks following AB discontinuation, previous levels of C. acnes were found, but those of Streptococcus were increased and those of Lactobacillus reduced versus baseline. Resistant C. acnes can develop.
The article by Bhate et al. BJGP 2021 reviewed the recurring issue of the association between long- term AB use for acne and antimicrobial resistance. This systematic review highlighted the lack of high- quality studies on this topic and the need for rigorous studies, since the rate of secondary infections, changes in the microbiota and rates of antimicrobial resistance remain unknown.
The median duration of acne treatment decreased from 11.5 months in 2003 to 126 days over the 2004-2014 period and 93 days over the 2008-2010 period.
Oral contraception: 30% decrease. ABs: 27% decrease.
Isotretinoin: 5% decrease.
Over the 2008-2016 period, dermatologist AB prescriptions decreased by 37%.
Maintenance treatments with topical agents
Spironolactone Oral contraception Isotretinoin
Infra-antimicrobial doses of doxycycline (40 mg vs 100 mg) Patient and prescriber education
Sarecycline: FDA approved in October 2018, narrow spectrum, limited action on gram+ intestinal bacteria and the intestinal microbiome. Better protection of the intestinal microbiome, little resistance.
Alternatives to long-term antibiotic therapy for acne are a key issue. New AB agents have demonstrated their efficacy and seem less likely to induce resistance, but long-term data are still lacking.
Speaker: Dr. Carina Woodruff
Report written by Dr. Rémi Maghia
During the “Contact Dermatitis” session, Carina Woodruff (San Francisco) gave an update on emerging allergens.
Preservatives: isothiazolinones are still a problem, ranking as the allergens most frequently found in patch tests after nickel.
While methylisothiazolinone (MI) and methylchloroisothiazolinone/methylisothiazolinone (MCI/MI) showed a decline over the 2011 to 2019 period, the rate of positive patch tests with benzisothiazolinone (BIT) increased from 0.26% to 3.43% in 2019.
The sources of exposure to BIT are particular: it is found in 16.4% of household and industrial products and is generally not contained in personal care products. Large amounts of BIT are found in cleaning products, detergents and paint. Contained in 94% of paints and often not declared, BIT has severe effects requiring hospitalisation (9%) and prednisone (27%), leading to mucosal symptoms (23%). Product emissions from a newly painted room last up to six weeks.
Other clinical presentations: dermatitis of the hands, widespread involvement (26%), face, head and neck, and rhinitis following airborne exposure.
There is a high rate of cross-reactions between MI and MCI, and up to 10% of patients sensitised to MI have also reacted to BIT.
Used as a moistening agent, vehicle and preservative, it is increasingly being used in cosmetics for sensitive skin such as body and face moisturisers.
It induces dermatitis of the face and skin folds, often in patients with AD or SD and often causing severe symptoms. There are no patch tests on the market.
Public concerns about preservatives such as parabens have led to the use of “para-preservatives”, reducing the use of traditional preservatives. They are found in essential oils, plant extracts and organic acids such as benzoic acid, which is not necessarily a good idea.
This is the most common sensitiser in fragrances according to several studies, with rates of positive patch test reactions ranging from 7 to 24%. Cross-reactions with other fragrance markers are limited (30 to 50%). Sources of linalool: linalool and limonene are the fragrances most frequently used in commercially sold topical products (personal care products including scalp products and fragrances). It is also found in foods, industrial beverages, cleaning products and essential oils (88%).
In products derived from cannabis, in addition to THC and CBD, terpenes including linalool and limonene are emerging.
It is ubiquitous.
Aluminium salts are found in 24 vaccines and some specific immunotherapies. Injection-site granuloma is the typical presentation. Other manifestations include “pseudo excited skin syndrome” (with patch testing), dermatitis of the hands and arms, and systemic contact dermatitis.
Pooled prevalence from seven studies was 1.48% (5.61% in children).
Patch testing uses 2% in petroleum jelly for children and 10% for adults. Reading on D7 is essential. Testing should be performed in plastic chambers.
Post-vaccination granuloma is not a vaccine contraindication! Some vaccines are aluminium-free. Intra-muscular injection can prevent granuloma (Barbaud et al., 2013). There are also aluminium-free immunotherapy options.
It can cause dermatitis of the shins, dyshidrosiform or hyperkeratotic refractory palmar-plantar dermatitis, or generalised dermatitis.
It is a by-product of ethyl vinyl acetate (EVA), used in sporting equipment (miscellaneous protective gear, shin pads, goggles, saddles, ski shoes, etc.). No commercial tests are available.
Speaker: Dr. Antonella Tosti
Report written by Dr. Rémi Maghia
In the “Therapeutic Hotline” session, Antonella Tosti (Miami) presented a number of new therapies in onychology.
The rationale for accelerating nail growth with minoxidil is increasing blood flow, with implications for onychomycosis and yellow nail syndrome.
Twice-daily application of topical minoxidil 5%: a pilot study showed an increase (in mm/month) in the growth rate of the treated nails. Similarly, positive results were obtained in a study evaluating yellow nail syndrome where it was combined with oral terbinafine, which is known to have this property.
Changes in growth were quantified, related the dose and duration of treatment, as were changes in terms of the thickness and hardness of the nail plate.
Preliminary results were obtained: a significant difference was observed in terms of nail solidity and growth. As for thickness, the observed increase was not statistically significant.
Multiple trials have been conducted proving the action of tofacitinib on psoriatic nails.
A meta-analysis showed that tofacitinib and ixekizumab were the molecules that provided the most improvement in nail scores in cases of psoriasis.
In a retrospective study including 33 patients with moderate to severe alopecia areata treated with oral tofacitinib, 73% showed nail improvement. This improvement occurred later than hair regrowth.
An article in JAMA 2021 showed a spectacular effect of tofacitinib as treatment for nail lichen planus associated with alopecia universalis.
Another article in JAMA 2022 showed complete improvement after six months when severe nail lichen planus was treated with baricitinib 4 mg/day, with a slight recurrence when baricitinib was reduced to 2 mg/day.
The main difficulty lies in recognising it. The presence of bleeding accompanied by an exposed nail bed are warning signs. Often, these patients come in with a large number of unnecessary treatments. In addition to podiatry treatments and behavioural therapies, Antonella Tosti mentioned the use of N- acetylcysteine, 1200 to 1800 mg/day. N-acetylcysteine is a glutathione and glutamate modulator. It restores levels of glutamate, a neurotransmitter, reducing compulsions and urges. A randomised controlled study in 42 children and adolescents with onychophagia showed a significant increase in nail length. Antonella Tosti published the success story of a 14-year-old adolescent with onychotillomania of both index fingers for two years who was treated for four months with N- acetylcysteine, 1800 mg/day.
Lastly, Antonella Tosti underlined the usefulness, in behavioural therapy, of smart bracelets, initially developed for trichotillomania. There are also behaviour-change websites, such as ONLINE-
TICS (publication in J Clin Med. 2022: ONLINE-TICS: Internet-Delivered Behavioral Treatment for Patients with Chronic Tic Disorders).
Speaker: Dr. Bianca Maria Piraccini
Report written by Dr. Rémi Maghia
In the "Hair loss from trichoscopy to therapy" session, Bianca Maria Piraccini (Bologna) presented the latest data on the use of topical finasteride (F) for male androgenetic alopecia (AGA).
F is a type-2 5-alpha-reductase inhibitor that in 1998, at the dose of 1 mg/day, was authorised by the FDA for the treatment of androgenetic alopecia in men aged 18 to 41. This means that for this indication, we have 20 years of hindsight concerning the efficacy and safety of F.
5-alpha-reductase inhibition reduces the conversion of testosterone into DHT. It should be noted that the effects of androgens on the hair follicle differ depending on the region: miniaturisation of scalp hair, transformation of vellus hairs into terminal hairs during puberty (beard, axillary folds, pubis). In young male subjects, finasteride can have a negative impact on beard growth. Sexual side effects are rare (below 2%) and reversible upon stoppage of the medication. Gynecomastia is very rare.
However, thanks to the Internet, public concerns about the risk of sexual effects have resulted in restrictions and criticisms, which may potentially be offset by proposing topical treatment.
The first test conducted with topical F dates back to 1997; in 2020, a literature review listed 33 articles on topical F for male and female AGA. In October 2021, in JEADV, Piraccini et al. published a multi- centre, randomised, double-blind, placebo-controlled study comparing topical F vs a placebo (with the same excipient) vs oral F 1 mg after 24 weeks in males with AGA.
At what concentration? 0.25%. What vehicle? Hydroxypropyl chitosan, a water-soluble semi-synthetic derivative of chitosan (chitin from the shells of crabs).
Topical application of F gave a mean maximum plasma concentration 100 times lower than that obtained with oral F 1 mg.
The study by Piraccini focused on men between the ages of 18 and 40 who had mild to moderate AGA. Topical F 0.25% was administered using a spray applicator with a plastic cone that prevented product dispersion in the air. Each actuation delivered 50 µl of solution, equivalent to 0.114 mg of F. One to four sprays were delivered in the morning and the solution was left in place for at least six hours.
Efficacy was evaluated at weeks 12 and 24 using standardised photos, with counting of hairs from 1 x 2 cm digital images over a tattooed area (primary endpoint). At W24, the increase in hair count versus baseline (20.2 vs 6.7 hairs) was significantly greater than with the placebo and was equivalent to that observed with oral F.
Safety in the topical F group was the same as in the placebo group and better than with oral F. The mean DHT concentration at W24 in the topical F group was lower than in the oral F group.
The product has been commercially available in Italy since May 2021.
In conclusion: when should it be prescribed?
Young adults
No need for beard growth Fear of systemic use Moderate AGA
Can be combined with minoxidil
Speaker: Prof. Pascal Joly
Report written by Dr. Rémi Maghia
During the "Autoimmune blistering diseases: what’s new?" session, I chose the presentation by Pascal Joly (Rouen), which focused on answering a number of questions that continue to be raised in clinical practice.
Dipeptidyl peptidase-4 inhibitors (gliptins)
These are increasingly being recognised for their association with BP. The time between their introduction and the onset of BP can be long, sometimes longer than one year.
It is difficult to issue clear recommendations as to whether or not gliptins should be discontinued, as studies investigating this issue have shown conflicting results, with some studies claiming that discontinuation has no benefits and with others affirming the opposite. However, we can recommend substitution with another diabetes medication.
Anti-PD1 and anti-PDL1 immunotherapies
In clinical practice, it is recommended to try to control BP lesions with therapies that do not reduce the anti-tumour efficacy of immunotherapy: for example, avoid high-dose corticosteroids (CSs) and conventional immunosuppressants when possible. We should try to continue immunotherapy for patients with mild to moderate BP, controlled with standard local or oral corticosteroid therapy. If BP is extensive or resistant, temporary stoppage of immunotherapy may be considered.
BP is a severe disease with a high mortality rate that increases with the use of high-doses oral CSs. Depending on the study, the one-year mortality rate ranges from 10-12 to 40% when high doses of oral prednisone are used. Two large meta-analyses confirmed that the one-year mortality of BP patients is three times greater than that of the general population of the same age and the same gender. The survival of BP patients depends on their age, general condition, and neurological and cardiovascular comorbidities.
The international multi-centre study of 311 BP patients conducted by Hébert et al. BJD 2021 evaluated the safety and efficacy of prednisone as initial treatment for BP at the dose of 0.5 mg/kg/day. Control of disease activity on D21 was 62 to 75% for mild to moderate BP and 46% for severe BP. At one year, the complete response rate was 38%, where only 11% had discontinued all treatment. One-year mortality was 17%. Predictors of good safety were: a Karnofski score above 70% and a negative predictive value for death of 94%. Factors for reasonable efficacy were: a BPDAI activity score ≤50 and a positive predictive value for disease control of 75%.
What should be done when a patient's disease is not controlled by an initial prednisone dose of 0.5 mg/kg/day? Two options: increase the dose to 0.75 mg/kg/day or add local corticosteroids 30 g/day (the most frequently chosen option).
Immunosuppressant drugs such as MTX, AZA and MMF are supposed to be steroid-sparing, but this has not been clearly demonstrated in the literature. A German RCT included patients receiving prednisone at the initial dose of 0.5 mg/kg/day + AZA 1.5 to 2.5 mg/kg/day. Only 18% of patients were able to reduce prednisone, which did not reflect a major therapeutic effect.
For MTX (12.5 mg/week) + topical clobetasol for one month vs a topical CS alone for nine months, the rate of relapse for MTX was 38% vs 67% for local corticosteroids. The rate of adverse effects was higher in the MTX group, leading to discontinuation in 54% of cases.
In conclusion, regarding the use of immunosuppressants for BP: Their indications remain unclear. They can be recommended: for patients with contraindications for oral CSs (diabetes, severe osteoporosis, significant cardiovascular problems). For BP relapses. For the few patients resistant to topical and oral CS treatment.
Tetracyclines: an RCT compared doxycycline 200 mg/day + topical CS vs prednisone 0.5 mg/kg/day. Success rates (without any switching from one group to the other, since the study was biased in this regard) were 54% vs 85%.
A large-scale real-life study (BJD 2021) showed that 72% of BP patients who started with tetracyclines also received prednisolone. Only 19% of BP patients did not need oral CSs and only 12% continued to be treated with doxycycline alone.
In conclusion regarding tetracyclines: they are mainly used in association with topical or oral CSs for mild to moderate BP. They can be tested for patients who are in poor general condition or have a contraindication for conventional immunosuppressants.
Dapsone: a German RCT with 54 BP patients concluded that dapsone as monotherapy enabled a small number of patients to stop using CSs. Moreover, dapsone can induce potentially serious side effects (anaemia, methaemoglobinaemia, neutropoenia, etc.). Therefore, a great deal of caution is required for elderly patients with cardiovascular comorbidities.
Rituximab
According to the 2021 update to the European guidelines: rituximab can be considered a non- validated option, due to concerns about the risk of serious and even fatal infections following B-cell depletion in elderly patients.
Omalizumab: it seems effective in particular for treating the acute stages of BP. It can be considered: for BP patients with urticarial inflammatory lesions and high IgE levels, who do not respond to oral or local CSs or who have contraindications for oral CSs, and for patients with neoplasia.
Speaker: Prof. Thierry Passeron
Report written by Dr. Rémi Maghia
The vitiligo session on the last day of the conference met with great success. I selected the presentation by Thierry Passeron (Nice), who was just as informative as usual and provided us with new information.
He reminded us that the treatment of vitiligo has three objectives: Stop melanocyte destruction
Induce melanocyte proliferation and differentiation (a long process requiring six to 24 months of treatment)
Prevent relapses
Some clinical signs can help determine whether vitiligo is active: hypochromic borders under Wood’s lamp, blurred borders, confetti-like depigmentation. When vitiligo is highly active, it should be treated urgently because it can spread very rapidly, making treatment more difficult.
How can a flare-up be blocked? Oral mini-pulse therapy with betamethasone or dexamethasone involves taking 5 mg for two days in a row every week (half-dose for children) for three to six months. This prevents the disease from spreading in over 85% of cases. The same results are achieved with low daily doses of oral prednisolone for two months, or with IV methylprednisolone pulse therapy for three days consecutively. A large retrospective study showed that with systemic corticosteroids (CSs), disease activity was stopped in 92% of cases. There are no randomised prospective placebo- controlled studies.
MTX, cyclosporine and minocycline also appear to be effective.
However, UVB TL01 phototherapy two or three times a week is also active in this phase and has the advantage of also inducing repigmentation. This demonstrates the relevance of combining narrow- spectrum UVB and mini-pulse therapy for highly active forms.
The role of oral JAK inhibitors in these active forms is not known.
CSs are equally effective with topical (preferred) and intra-lesional (more likely to induce atrophy) administration. Potent topical CSs are just as effective as highly potent CSs but are preferred because they have fewer side effects.
Topical calcineurin inhibitors (off-label use)
They are just as effective as topical CSs. Tacrolimus 0.1% is superior to 0.003%; it should be applied twice daily. Its efficacy is reinforced by UV rays, e.g. natural UV rays.
The combination of phototherapy and topical CSs
An RCT showed that the UVA-fluticasone propionate combination performed better than UVA therapy or topical CSs alone.
The combination of phototherapy and calcineurin inhibitors It performs better than calcineurin inhibitors alone.
With regard to combination therapies, it should be noted that they are currently the gold standard. They enable the face to be repigmented in 70 to 80% of cases. However, the patient (and dermatologist) needs to be aware that it requires six to 24 months of patience!
A new promising therapy: gastro-protected SOD
Antioxidants help combat oxidative stress, which plays a role in vitiligo. However, not all have the same efficacy and the digestive process breaks them down.
Superoxide dismutase (SOD) was recently studied (2021 publication in JEADV): a prospective, randomised, double-blind, placebo-controlled study at Nice University Hospital focused on 50 patients with long-standing or resistant vitiligo affecting over 5% of body surface area. Patients received GP- SOD 500 mg twice daily for three months followed by 500 mg once daily for three months or the placebo. All underwent twice-weekly UVB therapy. The percentage repigmentation evaluated by the VES score showed that the SOD group was significantly more repigmented (20% vs 9%). There were no side effects and safety was excellent.
Topical ruxolitinib is a JAK inhibitor that was recently studied as a 1.5% cream for the treatment of vitiligo. Efficacy on the face: over 57% of patients had repigmentation above 50% after one year, while one-third had repigmentation above 90%. Efficacy on the body was slightly lower. It should be noted that these very significant results were achieved without UV rays and that this treatment will probably be even more effective if combined with UVB therapy.
Over 40% of lesions become depigmented again in the year following treatment. The first treatment that has proven effective for preventing vitiligo relapses is topical tacrolimus 0.1% twice weekly. This was proven by a prospective, randomised, double-blind, placebo-controlled bi-centre study, J Invest Dermatol 2015.
Active forms of vitiligo should be treated as emergencies. Relevance of mini-pulse CSs + UVB therapy for active forms. The repigmentation of vitiligo takes six to 24 months.
Relevance of combination therapies: UVB rays (or sun exposure) + topical treatments + oral antioxidants.
New treatments are being developed, in particular topical and oral JAK inhibitors, some of which will probably be available soon.