Share
1
item
избран
Получете достъп до изключителни дерматологични услуги, за да подобрите своите професионални знания: над 500 визуални материала за патологии, клинични случаи и експертни видеа
Възползвайте се от ценни функции: аудио слушане, материали за споделяне с вашите пациенти
Бъдете информирани за предстоящи събития и уебинари, последни научни публикации и продуктови иновации
Вече имате профил? Влезте тук
Reports written by Dr. Marie Eve Pinet (Dermatologist, Quebec) and Dr. Nicolas Kluger (Dermatologist, Finland)
Related topics
Speakers :
Report written by Dr. Marie Eve Pinet
We had the opportunity to listen to several speakers during this session.
First of all, Dr Angelo Marzano spoke about the role of autoinflammation in syndromic hidradenitis suppurativa (HS). Autoinflammatory diseases are a group of diseases that present as recurring episodes of inflammation in various organs. They can take various forms when they affect the skin. These include neutrophilic dermatoses, which can appear as pustules and skin abscesses, for example. The main syndromes that can include hidradenitis suppurativa as one of the possible manifestations are SAPHO, PASH and PAPASH (others?). The study of these diseases, particularly in the context of HS, highlights the role of several genes that could lead to the selection of more targeted and patient-specific treatments. These genes include a loss-of-function mutation in OTULIN, responsible for cutaneous and gastrointestinal disorders, and AIM2. Syndromic HS can thus be characterised as a polygenic autoinflammatory disease and studies point to a correlation between its genotype and phenotype.
Secondly, Dr Vincenzo Bettoli talked about the correlation between HS phenotypes and acne. It is not always easy to distinguish between acne in HS and acneiform HS, which can occur in typical acne sites. However, this distinction can be particularly important as these are different diseases: acne is a disorder of the pilosebaceous unit whereas HS involves the terminal hair follicles. Therefore, they can respond differently to the treatments offered, i.e. acne will be more effectively controlled with isotretinoin whereas a biological agent will be more effective against HS. There are even cases where HS is aggravated by isotretinoin, but this is not specific to acneiform HS. Distinguishing between these conditions is easier in mild cases according to current data. Patients with acneiform HS are more likely to have fistulae, plaques, bridge scars and an irregular distribution, although these features are not exclusive to them.
Next, Dr Natalia Kirsten presented data from the German HS-Best registry regarding the frequency and predictors of inflammatory bowel disease (IBD) in patients with HS. The link between HS and IBD has often been described. Indeed, the risk of IBD is significantly higher in patients known to have HS than in the general population. Nevertheless, few studies have investigated the factors that could predict the risk of IBD in this specific population. Overall, the prevalence of IBD in patients with HS is close to 4%; it is higher for Crohn’s disease. The most recent data suggest that being female and having a larger number of chronic inflammatory comorbidities are the two significant factors that can predict the risk of developing IBD. Dr Kirsten’s study also found a connection between the presence of HS lesions on the chest and IBD. Consideration of potential IBD is important for HS patients given the potential for gastrointestinal deterioration with the introduction of an anti-IL17 biological agent in this population.
Dr Anne-Sophie Sarkis briefly presented the data and scores of Belgian patients from the European Registry for Hidradenitis Suppurativa (ERHS). This registry collects a wide range of data through extensive questionnaires and calculates a total of nine scores. Of the 609 patients, some even have a syndrome associated with HS. The information compiled and analysed has highlighted certain factors associated with a more severe disease, i.e. male gender, North African origin and HS-related depression. These data can help us better understand the disease and provide the most personalised treatments possible.
Dr Antonio Martorell described the phenotypes of HS based on elementary lesions. The question that was put forward was whether it is possible to predict which patients are at risk of HS progression according to the initial evaluation. The main phenotypes described are the follicular and inflammatory types, where the former is primarily characterised by comedones and the latter by abscesses and sinus tracts. The follicular phenotype appears to have the potential to progress to a mixed form, more often in men. It seems that the triggers may include chronic smoking and a body mass index above 30 as well as eating habits and a stressful event. Predicting the progression of the follicular form may be useful in particular for surgery, which can be much less aggressive if performed early. Some tools, such as ultrasound and genetic analysis, could help assess the probability of progression.
From a genetic point of view, Dr Cécile N. Meddour went on to demonstrate the importance of cutaneous pluripotent stem cells in understanding the role of PSENEN mutations in HS. Studying these mutations could facilitate the development of more targeted treatments.
Lastly, Dr Sophie Hue presented the genetic analyses of 100 patients with familial or sporadic HS, performed using whole exome sequencing. The presence of certain mutations already described in the literature was demonstrated, along with others that had not yet been described in relation to the γ-secretase complex. It should be noted that two genes are involved in obesity and tobacco sensitivity.
Speakers:
Report written by Dr. Marie Eve Pinet
This conference featured several speakers who spoke about a variety of treatments.
Firstly, Dr Zouboulis presented current data on TNF inhibitors. We currently know that hidradenitis suppurativa (HS) combines altered follicular keratinocyte differentiation and inflammation. All this seems to take place in progenitor cells. Studies also suggest that TNF-α is one of the main cytokines increased in blood, lesional and perilesional skin in patients with HS, although it is not a specific marker. Adalimumab is therefore a logical option in the therapeutic arsenal for HS, with a reduction in inflammatory nodules and abscesses. However, analyses do not show a decrease in TNF-α expression in the skin or in its serum concentration, although ex-vivo studies have shown a decrease in its concentration in cultured lesional tissue. Nevertheless, the molecule does not appear to improve the control of drainage tunnels under the skin. Other factors contributing to the disease include the role of adipose tissue, genetic susceptibility, inflammatory mediators associated with smoking, pro-inflammatory signals associated with obesity, and the composition of the microbiome. In HS patients, studies have also shown that IL-17 plays a role in the activity of this condition. Therefore, in some cases, it would clearly be beneficial to treat patients with drugs such as secukinumab and bimekizumab. However, these options still need to be studied further.
Secondly, Dr Straalen spoke about the current guidelines for the treatment of HS. Today, we are generally advised to use tetracyclines for mild to moderate forms and then a combination of clindamycin and rifampicin or else start with this combination for more severe forms. If this fails, the next step is to use a biological agent. However, the evidence for the efficacy of these treatments is limited and the origin of their effects is not yet clear. The most recent review of the data, however, suggests that tetracyclines could be a first-line choice in moderate to severe cases, particularly in TB-endemic areas or for patients with contraindications such as drug interactions. Even low-dose doxycycline could be an option to consider. Moreover, studies suggest that clindamycin could be effective as monotherapy, particularly for mild to moderate forms of HS, although combining it with rifampicin could remain useful for moderate to severe cases.
Dr Rosi presented data on the efficacy of PDT with the photosensitiser RLP068/Cl in the localised treatment of HS lesions. The options evaluated included topical and intralesional PDT. In the study presented, patients tolerated the PDT treatment well, with minor and transient side effects including erythema. It appears that PDT can selectively destroy the affected cells in HS, stimulate the inflammatory response, kill bacteria, and break down biofilms. It can also rapidly reduce the pain associated with skin lesions and does not appear to have the ability to induce bacterial resistance.
Dr Ohm spoke about switching from adalimumab originator to a biosimilar. In the study presented, one third of the patients who made the switch developed side effects and/or had loss of response to treatment. However, these effects did not seem to occur with the treatment of other conditions such as psoriasis, arthritis and inflammatory bowel disease. Further studies are needed, but the current results suggest that switching to a biosimilar exclusively for cost reasons is not advisable.
Lastly, Dr Ramirez presented the results of an analysis concerning the use of metformin in HS. The mechanism is not completely clear for the time being, but it seems that patients with signs of hyperandrogenism could benefit from this molecule, which appears to have significant anti-inflammatory effects. Indeed, it may reduce the secretion of TNF-α and IL-17. The results presented during this presentation indicated that in general, patients continued treatment for a median period of 12 months and that the risk factors for discontinuation of the medication were male gender, smoking, and HS lesions on the abdomen.
Speakers:
Report written by Dr. Marie Eve Pinet (Dermatologist, Quebec)
During this conference, the presenters discussed various treatments.
First of all, Dr Reguiai presented the results of the Phase 3 SUNSHINE and SUNRISE studies on the use of secukinumab for moderate to severe hidradenitis suppurativa. Overall, these studies strongly suggested that early intervention may slow down the progression of the disease and reduce its severity. In both studies, the drug was found to provide a superior clinical response to the placebo at week 16 in Hurley stage II and III patients. Administration every two weeks resulted in greater improvement in skin pain at week 16 and was more effective at controlling flare-ups in Hurley stage III patients than the placebo. Hurley stage II patients tended to have a better response to secukinumab than stage III patients. Lastly, the data indicated that the drug was well tolerated and had a good safety profile.
Dr Zouboulis then went on to present a post-hoc analysis of the SUNSHINE and SUNRISE studies that was based on the IHS4 score. This score enables HS to be evaluated in terms of severity and assigns a value to the various types of possible lesions. It showed that secukinumab led to a rapid improvement in the IHS4 score that for some patients started after two weeks and continued through to week 16. Achievement of IHS4-55, IHS4-75 and IHS4-90 at week 16 was higher in the patients who received secukinumab than in those who received the placebo. An analysis of the data also showed high agreement between the IHS4-55 and HiSCR scores.
Dr Tzellos presented data from a Phase 2 study evaluating the efficacy of bimekizumab in HS patients. Compared with the placebo, a higher proportion of patients receiving bimekizumab achieved IHS4-55 (almost 57% of the study group, compared with 15% in the group receiving the placebo). There was also a significant proportion of patients achieving IHS4-55 who had a decrease in skin pain and the DLQI. In addition to these findings, this study showed the relevance of IHS4-55 as an effective and dynamic measure of treatment efficacy for moderate to severe HS. It should be noted, however, that Phase 3 studies will need to be conducted to confirm these results with a larger number of patients.
Dr Aarts presented the results of a study comparing the use of adalimumab in combination with surgery or as monotherapy in a real-world setting. The resulting data showed a faster decrease in disease severity after 12 months when patients were treated with a combination of adalimumab and surgery; quality of life also significantly improved. This study had high external validity and presented a good option for patients with multiple skin tunnels. However, both groups had a high treatment discontinuation rate (20%) and there were many missing values with regard to the HiSCR scores. Moreover, the context of the COVID pandemic was likely another limitation of this study.
Next, Dr Van der Zee presented the results of a post-hoc analysis of the data from the SUNSHINE and SUNRISE studies on the impact of secukinumab administration on the need for rescue surgery in patients with moderate to severe HS. The interventions taken into account included incisions, the drainage of lesions, and local excisions. According to the data obtained in both studies, the rate of implementation of such interventions was low at week 16 of secukinumab administration. In addition, the need for rescue treatment, whether surgical or medical, was lower despite a more severe baseline disease. This analysis also confirmed that the treatment was well tolerated and safe. It would be useful to observe secukinumab-treated patients over longer periods of time to further assess this drug’s ability to reduce the need for rescue interventions for painful acute lesions.
Lastly, Dr Kirby presented data from a Phase 2 study on the administration of povorcitinib, a Janus kinase 1 inhibitor, for HS patients. The analysis suggested an improvement in the condition of patients who were switched from the placebo or a lower dose to 75 mg/day of povorcitinib. Moreover, at this dose, the improvement observed was long-lasting and up to almost 30% of patients achieved HiSCR100 or IHS4-100 with this dose level. Patients tolerated the medication well throughout the 52-week study. A Phase 3 study is currently in the recruiting phase to compare the administration of povorcitinib or a placebo in patients with moderate to severe HS.
P-009 Fougerousse AC, et al. Characteristics of patients with paediatric onset hidradenitis suppurativa
P-087 Mora-Fernández V, et al. Paediatric hidradenitis suppurativa: follow-up after 6 years. A descriptive study.
Report written by Dr. Nicolas Kluger
Epiver was a French multi-centre community-hospital study carried out between March 2016 and December 2017 (P-009). The members of the RésoVerneuil network anonymously recorded data from a standardised evaluation of their HS patients. A total of 1428 patients were included. Of them, 528 had a disease with paediatric onset and 856 with adult onset. On average, in the group of children, the symptoms of HS had started at the age of 14.5. The average diagnostic delay was 9.6 years in the group of children. The patients in the paediatric group were more likely to have a family history of HS (p=0.024) or pilonidal sinus disease (p=0.011). Cannabis use, BMI, Hurley stages and impact on quality of life were similar. Patients with paediatric onset HS were more likely to have involvement of the inguinal folds (p=0.029), breast area (p=0.013), face (p=0.006), torso (p=0.015) and legs (p=0.02). Those with adult onset HS more frequently had HS lesions in the genital area (p=0.004) and on the scalp (p=0.036). Patients with adult disease were more likely to have inflammatory bowel disease (p=0.004), dyslipidaemia (p<0.001) and diabetes mellitus (p<0.001). Pilonidal sinus disease, acne, chronic inflammatory rheumatism and hypertension were comparable between the two groups.
Key takeaways: the frequency of a family history of HS in paediatric forms; the long diagnostic delay in France (nine years), and the different clinical forms between paediatric onset and adult onset HS.
Moreover, a small-scale Spanish study evaluating 12 children with HS showed that the development of HS in childhood was not a predictive factor for progression or improvement of the disease (P-087).
P-178 Medianfar CE, et al. Hidradenitis suppurativa and female infertility: a cross-sectional pilot study.
Report written by Dr. Nicolas Kluger
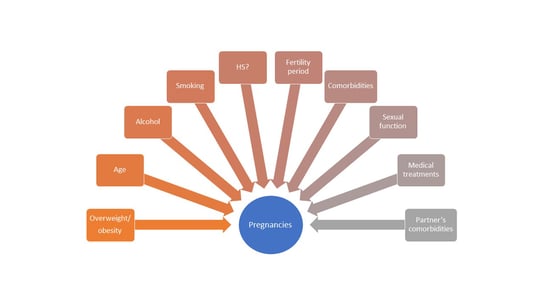
The connection between polycystic ovary syndrome (PCOS) and HS is well known. PCOS is often associated with infertility or reduced fertility. Current studies on HS and infertility suggest a correlation, but the data are limited. A Danish study included 161 women (55 with HS, 55 with another dermatosis and 51 healthy controls). The following information was collected: pregnancies, deliveries, abortions, in vitro fertilisation, other factors known to have an impact on fertility (smoking, PCOS, thyroid disease, methotrexate treatment and comorbidities in male partners, Figure). The sexual function of the participants was evaluated using the Female Sexual Function Index (FSFI). Infertility was defined as failure to conceive after >12 months of regular sexual intercourse in the absence of contraception.
In the end, no significant differences were found between the three groups in terms of having or not having children, the number of pregnancies, or infertility. For those who had children, no significant difference was found with regard to the number of children.
This study was therefore reassuring for women of childbearing age with HS, although the limitations inherent in its design should be taken into account.
Figure. Factors influencing fertility and therefore the ability to conceive.
P-040 Isra N, et al. Colonoscopy findings in hidradenitis suppurativa
Report written by Dr. Nicolas Kluger
The connection between inflammatory bowel disease (IBD), especially Crohn’s disease, and HS is well known. Dermatologists from Mayo Clinic in Rochester reviewed the records of 98 patients with HS and 65 patients with both HS and IBD who had had a colonoscopy. Unsurprisingly, mostly only patients with HS + IBD had abnormal colonoscopy findings (erythematous colonic mucosa, ulceration, stricture, fistula). However, the authors reported that 20% of the patients with HS described digestive symptoms (vomiting, diarrhoea, abdominal pain).
The key point to remember here is that in the event of perianal lesions, colonoscopy can help distinguish between isolated HS and HS with IBD. However, the poster was not particularly clear. Not much additional information was given concerning the prevalence of digestive symptoms or the investigations carried out for the 20% of patients with HS and digestive disorders with normal colonoscopy: for example, information was lacking with regard to the role of macroscopically normal mucosal biopsies, gastro-duodenal fibroscopy and biological testing for faecal calprotectin for example.
P-002 Lee JH, et al. Epidemiology and Comorbidity of Hidradenitis Suppurativa in Korea for Years: A Korean Nationwide Population-based Cohort Study
P-005 Knecht-Gurwin K, et al. Prevalence of hidradenitis suppurativa in Poland
P-011 Broboel A, et al. Prevalence and epidemiology of patients with Hidradenitis suppurativa in the Faroe Islands
P-012 Gaspard S, et al. Prevalence of hidradenitis suppurativa: results from the French team of the GHiSA project.
Report written by Dr. Nicolas Kluger
Several national posters evaluated the prevalence of HS. In the Faroe Islands, it is estimated at 0.1% and affects women in 78% of cases (P-011). In Poland, it is 1.5% but primarily affects men (in 67% of cases) (P-005). In France, a study conducted as part of the Global Hidradenitis Suppurativa Atlas (GHiSA) found a higher prevalence rate than in the past (3.4-3.6%) (P-012). In South Korea, the overall prevalence of HS rose from 0.03% to 0.14% between 2003 and 2019. The incidence and prevalence of HS increased in all age groups. Male predominance in HS was clear in Korea (P-002).
S-07-03 Fougerousse AC, et al. Hidradenitis suppurativa in transgender patients: a case series
Report written by Dr. Nicolas Kluger
Cases of HS in transgender patients are rare in the literature. Three cases of HS reported in the literature have involved male transgender patients. The RésoVerneuil group collected data on a series of six patients, aged 17 to 48 years, including four transgender women and two transgender men. None of the patients had a family history of HS or obesity. In four cases, HS developed following initiation of hormone therapy. In one case, HS improved and there were no flare-ups after the patient was put on testosterone. This was a heterogeneous series and it should be noted that, regardless of the type of hormone therapy, exacerbation is possible in the majority of cases. More cases involving transgender patients are needed in order to better establish the profile and course of the disease.
P-142 Alavi A, et al. Secukinumab in Moderate to Severe Hidradenitis Suppurativa: Analysis of Pooled Data from the SUNSHINE and SUNRISE Phase 3 Randomised Trials
Report written by Dr. Nicolas Kluger
SUNSHINE and SUNRISE were identical, multi-centre, randomised, placebo-controlled, double-blind phase 3 trials that aimed to evaluate the efficacy of secukinimab, an anti-interleukin-17 monoclonal antibody, in patients who had had moderate to severe HS (defined as a total of ≥5 inflammatory lesions affecting ≥2 different anatomical areas) for at least one year. In both trials, patients were randomised (1:1:1) to receive subcutaneous secukinumab 300 mg, every two weeks (SEQ2W) or every four weeks (SEQ4W), or a placebo (PBO). At week 16, patients previously randomised to receive either SECQ2W or SECQ4W continued with the same dosing regimen, while those randomised to receive PBO were switched to receive SECQ2W (placebo-SECQ2W) or SECQ4W (placebo-SECQ4W) until week 52 (figure).
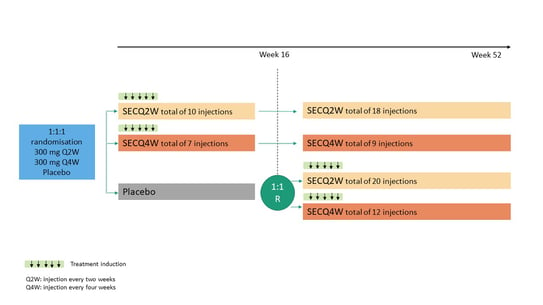
Figure title: SUNRISE and SUNSHINE study protocol
The primary endpoint was the proportion of patients with a clinical response, defined as a 50% or greater decrease in the number of abscesses and inflammatory nodules, with no increase in the number of abscesses or draining fistulas versus baseline, at week 16, as assessed in the overall population. HS clinical response was calculated based on the number of abscesses, inflammatory nodules, draining fistulas, total fistulas, and other lesions in the affected areas.
676 patients were selected for inclusion in the SUNSHINE trial and 687 for the SUNRISE trial, for a total of 1084 patients.
Secukinumab resulted in a higher proportion of patients achieving HiSCR than the placebo at week 16 (SECQ2W [43.7%]; SECQ4W [43.9%] vs placebo [32.4%]), with a trend towards improvement through to week 52 (SECQ2W [61.0%]; SECQ4W [59.2%]). Rapid improvements in HiSCR rates were also observed in patients switched from PBO to secukinumab at week 52. Benefits were observed for both dosing regimens compared with PBO in the secondary efficacy outcome measures (number of abscesses and inflammatory nodules, flare-ups, pain score, AN50 response) at week 16. The efficacy of SECQ2W and SECQ4W observed at week 16 was maintained until week 52 with a trend towards improvement. Quality of life was improved compared with PBO and this was maintained through to week 52.
The most frequent adverse events were headaches, nasopharyngitis, and worsening of HS. Moreover, three cases of de novo inflammatory bowel disease were observed. Candidiasis affected 4 to 6% of patients.
Thus, treatment with secukinumab Q2W or Q4W was effective with a favourable safety profile in patients with moderate to severe HS. Signs of efficacy were rapidly observed with the SECQ2W and SECQ4W treatments and the effect was maintained through to week 52 of treatment.
P-107 Martora F, et al. Paradoxical hidradenitis suppurativa induced by adalimumab biosimilar successfully treated with guselkumab in a psoriasis patient
P-098 Burzi, et al. Guselkumab in the treatment of severe hidradenitis suppurativa, a promising role?
P-187 Liakou AI, et al. Paradoxical reactions during treatment with biological agents: reports of 3 cases
P-038 Tampouratzi et al. Paradoxical skin reaction after anti-TNF treatment for inflammatory bowel disease: should we include hidradenitis suppurativa?
P-117 Salvia G, et al. A patient with hidradenitis suppurativa and psoriasis treated with Brodalumab who developed pyoderma gangrenosum: a paradoxical reaction?
Report written by Dr. Nicolas Kluger
A paradoxical reaction can be defined as the development of a new inflammatory disease during the treatment of a first one with a biotherapy. The paradoxical effects of TNF-alpha inhibitors in psoriasis are now well known. Psoriasiform reactions in HS patients treated with TNF-alpha inhibitors are also known.
Martora et al. (P-107) reported the case of a 25-year-old woman with psoriasis who developed paradoxical HS 16 weeks after starting a TNF-alpha inhibitor (adalimumab). She was then treated with guselkumab, an IL-23 inhibitor, which led to remission of her psoriasis and improvement (but not disappearance) of her HS. The authors questioned the role of IL-23 in the pathophysiology of HS, especially since IL-23 is hyperexpressed in macrophages in HS lesions. Another Italian poster (P-098) reported the efficacy of guselkumab in a woman who had not responded to adalimumab and also had paradoxical psoriasis induced by the TNF-alpha inhibitor.
Several cases of paradoxical psoriasis during treatment with TNF-alpha inhibitors for HS (P-187) have been effectively treated with secukinumab (IL-17 inhibitor).
The development of cases of HS during treatment with TNF-alpha inhibitors in patients with chronic inflammatory bowel disease also raises the issue of paradoxical reactions in these patients (P-038).
Lastly, it can be noted that a case of pyoderma gangrenosum was observed in a patient with psoriasis and HS treated with an IL-17 inhibitor (P-117).
These observations illustrate the complexity and intricacy sometimes observed in cases of primary inflammatory dermatoses or those paradoxically induced by treatments.
P-127 Ezanno AC, et al. Does BMI influence healing after hidradenitis suppurativa surgery?
P-128 Ezanno AC, et al. Influence of smoking on healing after HS excisions.
Report written by Dr. Nicolas Kluger
The same French team from Bégin Military Teaching Hospital reported about their experience with 160 patients. The first part of the French single-centre retrospective study (P-127) included 160 patients. It showed that obesity (BMI>30) was not associated with a longer time to complete healing than for patients without obesity. However, the time to healing was longer when comparing the overweight group with the normal weight group.
In the second part, they evaluated whether smoking had an impact on the time to healing, depending on the location: axillary, inguinal-perineal or other excision. It showed that smokers had a higher likelihood of healing than non-smokers, whatever the stage of the disease or the treatment. These results are more than surprising, especially as they were confirmed by a multivariate analysis. A centre effect and the use of different surgical techniques versus other centres cannot be ruled out. Further studies are needed.
P-106. Fougerousse AC et al. Retinoid use for hidradenitis suppurativa: a practice survey
Report written by Dr. Nicolas Kluger
The international guidelines on the management of HS differ depending on the retinoid and the HS phenotype. In France, there have been national guidelines since 2019.
The RésoVerneuil group reviewed the practicalities of prescribing retinoids for HS in France by conducting an online survey of the network’s members (278 members). Doctors were asked what retinoids were used in practice for HS and for what patient profile (follicular or classic, Hurley stage, gender); they were also asked how these retinoids were prescribed. A total of 107 responses were collected: 41 said they did not prescribe retinoids due to a lack of eligible patients (29.3%), a lack of experience (39%), or a lack of evidence in HS (61%). Of the 66 doctors prescribing retinoids, 61 used them for the "follicular" phenotype of HS and 12 for the "classic" form. The main retinoids used were isotretinoin (n=49), acitretin (n=39) and, less often, alitretinoin (n=9). Isotretinoin and alitretinoin were used as short-term treatment by around 40% of the doctors, unlike acitretin, which was mostly used as long-term treatment.
Retinoids were used after failure of antibiotics (n=57) and only rarely as first-line treatment (n=15); they were primarily used as monotherapy (n=27), or in combination with an antibiotic for flare-ups (n=42), sometimes with long-term antibiotics (n=14), with zinc (n=7), with surgery (n=20), or with a biotherapy (n=9).
In conclusion, >60% of doctors have prescribed retinoids for HS, mainly for the follicular phenotype. Isotretinoin and acitretin are the treatments prescribed, although the French guidelines consider all three molecules with the same level of evidence for follicular HS after antibiotic failure. Studies are needed to better clarify the role of retinoids in the treatment of HS.
P-154. Nilausen B, et al. Determinants of appointment absenteeism at a tertiary Hidradenitis Suppurativa outpatient clinic
Report written by Dr. Nicolas Kluger
Little is known about the factors associated with absenteeism in HS patients. A Danish single-centre study reviewed the demographic and clinical factors contributing to appointment absenteeism at an outpatient clinic.
Out of a total of 161 consecutive appointments scheduled for patient follow-up at the clinic, 37 (23%) patients were absent. The patients most at risk of absenteeism were men (p=0.028) of non-Caucasian origin (p=0.008). Patients with a family history of HS were less likely to be absent (p=0.004). However, the severity and clinical manifestations of the disease had no influence. These factors can be taken into account in the prevention of absenteeism; however, this study can be criticised for lacking substance: lack of a control group, usual rate of absenteeism at this clinic, consideration of the reasons for being absent, consideration of socio-economic factors, and the other comorbidities that may have been involved (psychiatric diseases, etc.).